nineteenth issue
September 21, 2022
Eosinophilic dermatosis of hematologic malignancy shows overexpression of T-cell type 2-related molecules
Journal of the American Academy of Dermatology
Th1 or Th2… and why you should care!
Eosinophilic dermatosis of hematologic malignancy (EDHM) occurs in patients with hematological malignancies such as lymphomas and commonly manifests as pruritic papules, nodules, and plaques. On histopathologic examination, there is dermal infiltration of lymphocytes and dermal-epidermal separation, resembling bullous pemphigoid (BP). Little is known about the role of Th2-related molecules in the pathogenesis of EDHM, so researchers sought to characterize T-cell signatures using immunohistochemistry.
This study analyzed skin biopsies and serum samples from 11 patients with EDHM, 11 patients with BP, and 5 healthy subjects that served as a control group. Researchers performed immunohistochemistry and found significantly higher levels of T-cell markers, including CD3, CD4, CD8, and CD5, in EDHM and BP skin compared to control. EDHM and BP samples also expressed significantly higher levels of IL-4 and IL-31 (Th2-related cytokines that recruit eosinophils and contribute to pruritus) compared to control. Lastly, researchers tested for the presence of T-bet and GATA3, which dictate master transcription of Th1 and Th2 cells, respectively. GATA3 (Th2 marker) cell density was significantly increased in EDHM and BP samples compared to control (p=0.01 and p=0.007, respectively). Conversely, T-bet (Th1 marker) density was similar between EDHM, BP, and control group, suggesting a predominantly Th2 response over Th1 response in EDHM and BP.
Limitations: This study used a relatively small sample size and a retrospective study design.
Main Takeaway: Immunohistochemistry comparisons suggest a predominantly Th2 immunity response in EDHM, indicating new potential therapeutic targets.
Eosinophilic dermatosis of hematologic malignancy (EDHM) occurs in patients with hematological malignancies such as lymphomas and commonly manifests as pruritic papules, nodules, and plaques. On histopathologic examination, there is dermal infiltration of lymphocytes and dermal-epidermal separation, resembling bullous pemphigoid (BP). Little is known about the role of Th2-related molecules in the pathogenesis of EDHM, so researchers sought to characterize T-cell signatures using immunohistochemistry.
This study analyzed skin biopsies and serum samples from 11 patients with EDHM, 11 patients with BP, and 5 healthy subjects that served as a control group. Researchers performed immunohistochemistry and found significantly higher levels of T-cell markers, including CD3, CD4, CD8, and CD5, in EDHM and BP skin compared to control. EDHM and BP samples also expressed significantly higher levels of IL-4 and IL-31 (Th2-related cytokines that recruit eosinophils and contribute to pruritus) compared to control. Lastly, researchers tested for the presence of T-bet and GATA3, which dictate master transcription of Th1 and Th2 cells, respectively. GATA3 (Th2 marker) cell density was significantly increased in EDHM and BP samples compared to control (p=0.01 and p=0.007, respectively). Conversely, T-bet (Th1 marker) density was similar between EDHM, BP, and control group, suggesting a predominantly Th2 response over Th1 response in EDHM and BP.
Limitations: This study used a relatively small sample size and a retrospective study design.
Main Takeaway: Immunohistochemistry comparisons suggest a predominantly Th2 immunity response in EDHM, indicating new potential therapeutic targets.
Lidocaine Ameliorates Psoriasis by Obstructing Pathogenic CGRP Signaling‒Mediated Sensory Neuron‒Dendritic Cell Communication
Journal of Investigative Dermatology
Journal of Investigative Dermatology
Lidocaine injection: a cute-aneous treatment option for psoriasis!
It is thought that both the immune system and the nervous system are involved in psoriasis, but current understanding of the neurogenic contributions remain unclear. Therefore, these authors wanted to see whether targeting the cutaneous nervous system could improve psoriasis. They conducted this pilot study where they injected lidocaine in the epidural space of patients with psoriasis. They found that:
Main Takeaway: Lidocaine epidural injection may be an effective treatment for patients with psoriasis through suppression of abnormal nerve growth and mediation of calcitonin and neuropeptide production from immune cells.
It is thought that both the immune system and the nervous system are involved in psoriasis, but current understanding of the neurogenic contributions remain unclear. Therefore, these authors wanted to see whether targeting the cutaneous nervous system could improve psoriasis. They conducted this pilot study where they injected lidocaine in the epidural space of patients with psoriasis. They found that:
- Lidocaine injection improved patient psoriasis scores (PASI scores)
- In a mouse model of psoriasis (induced by imiquimod injection), lidocaine improved skin lesions and inflammation. Lidocaine was even found to be as effective as a TNFa blocker in skin lesions, which is a current therapy for psoriasis
- In the mouse model of psoriasis, lidocaine improved psoriatic lesions through inhibition of abnormal cutaneous nerve growth and neuropeptide release
- In patients with psoriasis, single cell RNA sequencing of dermal immune cells identified increased calcitonin gene-related peptide receptors. Lidocaine inhibited IL-23 production by blockage of calcitonin gene-related peptide signaling from neurons to immune cells
Main Takeaway: Lidocaine epidural injection may be an effective treatment for patients with psoriasis through suppression of abnormal nerve growth and mediation of calcitonin and neuropeptide production from immune cells.
Is routine laboratory testing in healthy young patients taking isotretinoin necessary – a critically appraised topic
British Journal of Dermatology
Role of Surgery after Remission of Nonsystemic Extensive Periorbital Basal Cell Carcinoma Treated by Vismodegib
Dermatologic Surgery
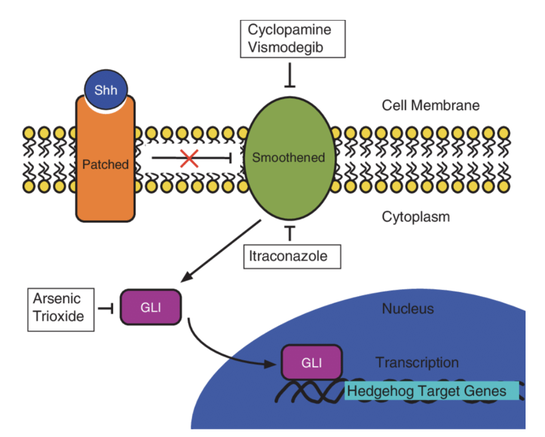
Vismodegib and surgery: the best team to defeat sonic the hedgehog (pathway)!
Basal cell carcinoma (BCC) is the most common skin cancer affecting the periocular area (the area around the eye), and usually is treated with surgery. However, in certain advanced or metastatic cases, surgery or radiotherapy may be contraindicated. In these cases, vismodegib is a medication that can be used for treatment by inhibiting the sonic hedgehog pathway, which is involved in the pathogenesis of BCCs. In recent studies, BCC remission rates with vismodegib ranging from approximately 20-40% have been reported. However, few studies have addressed the need for complementary resection or local reconstruction after medical treatment. This systematic review investigates the role of surgery in managing advanced periocular BCC. Researchers reviewed outcomes for patients with BCC around the eye treated with vismodegib alone, vismodegib + surgery, vismodegib + surgery + radiotherapy, and vismodegib + radiotherapy.
Basal cell carcinoma (BCC) is the most common skin cancer affecting the periocular area (the area around the eye), and usually is treated with surgery. However, in certain advanced or metastatic cases, surgery or radiotherapy may be contraindicated. In these cases, vismodegib is a medication that can be used for treatment by inhibiting the sonic hedgehog pathway, which is involved in the pathogenesis of BCCs. In recent studies, BCC remission rates with vismodegib ranging from approximately 20-40% have been reported. However, few studies have addressed the need for complementary resection or local reconstruction after medical treatment. This systematic review investigates the role of surgery in managing advanced periocular BCC. Researchers reviewed outcomes for patients with BCC around the eye treated with vismodegib alone, vismodegib + surgery, vismodegib + surgery + radiotherapy, and vismodegib + radiotherapy.
What did they find?
Limitations: This review was limited by the general lack of high-quality studies with study designs that overestimate efficacy.
Main Takeaway: While vismodegib is a reasonable option for neoadjuvant treatment for locally advanced periocular BCC, or in metastatic patients, surgery may play a bigger role than previously thought in confirming complete response to treatment, removing residual tumor or reconstructing the eyelid. In fact, the results from this review suggest that vismodegib + surgery may have the best results for achieving complete remission.
- 21 articles were selected for inclusion with 384 patients
- Overall, there was a significant complete clinical response in 37% (141/384) of patients after vismodegib treatment for mean of 36.7 weeks for nonmetastatic patients
- Rate of complete remission was upgraded by 6% when visomedigib was associated with surgery and 1% with the combo of vismodegib + surgery and radiotherapy
- Level 1 evidence= vismodegib as neoadjuvant therapy in locally advanced BCC that is not amenable to surgery and/or radiotherapy
- Level 3 evidence= role of surgical excision of residual clinically suspicious lesions after medical treatment
Limitations: This review was limited by the general lack of high-quality studies with study designs that overestimate efficacy.
Main Takeaway: While vismodegib is a reasonable option for neoadjuvant treatment for locally advanced periocular BCC, or in metastatic patients, surgery may play a bigger role than previously thought in confirming complete response to treatment, removing residual tumor or reconstructing the eyelid. In fact, the results from this review suggest that vismodegib + surgery may have the best results for achieving complete remission.