THIRTEENTH ISSUE
June 29, 2022
Sk(in depth) scoop
Just another kinase… or is it? Alopecia areata (AA) is an immune mediated form of hair loss, affecting approximately 2% of individuals. On June 13, 2022 the FDA released groundbreaking news: baricitinib (Oluminant) became the first FDA approved systemic therapy for adults with severe alopecia areata.
Baricitinib, a janus kinase (JAK) inhibitor, blocks the activity of a class of enzymes implicated in a number of inflammatory pathways. Previously approved to treat rheumatoid arthritis, the drug has also proven safe and efficacious for alopecia areata. In two randomized, double-blind, placebo-controlled trials published in The New England Journal of Medicine, over 1,000 patients were treated with either placebo, 2 mg Baricitinib, or 4 mg Baricitinib.
What did they find?
Main Takeaway: Though alopecia areata remains a challenging and unpredictable disease, FDA approval of baricitinib marks a monumental step towards providing patients with alopecia areata safe and effective treatment options. In the words of Nicole Friedland, President of the National Alopecia Areata Foundation, “This is the dawn of a new era. For the first time, alopecia areata patients have the option of an approved treatment that has undergone rigorous testing in clinical trials. We anticipate more treatments to come, bringing additional choices to our community.”
Baricitinib, a janus kinase (JAK) inhibitor, blocks the activity of a class of enzymes implicated in a number of inflammatory pathways. Previously approved to treat rheumatoid arthritis, the drug has also proven safe and efficacious for alopecia areata. In two randomized, double-blind, placebo-controlled trials published in The New England Journal of Medicine, over 1,000 patients were treated with either placebo, 2 mg Baricitinib, or 4 mg Baricitinib.
What did they find?
- By week 36, 22% of patients treated with 2 mg Baricitinib and 35% of patients treated with 4 mg Baricitinib achieved at least 80% scalp coverage, compared with only 3% who received placebo
- Safety data is also promising, with mostly minor side effects reported including upper respiratory tract infection, headache, acne, urinary tract infection and high cholesterol
- With long term use, the medication may still carry a risk of serious infections, malignancy, and major adverse cardiac events.
Main Takeaway: Though alopecia areata remains a challenging and unpredictable disease, FDA approval of baricitinib marks a monumental step towards providing patients with alopecia areata safe and effective treatment options. In the words of Nicole Friedland, President of the National Alopecia Areata Foundation, “This is the dawn of a new era. For the first time, alopecia areata patients have the option of an approved treatment that has undergone rigorous testing in clinical trials. We anticipate more treatments to come, bringing additional choices to our community.”
Atopic dermatitis is associated with shorter stature, higher BMI, and lower weight in kiddos
JAMA Dermatology
JAMA Dermatology
How do you get rid of an itch? Start from scratch. Atopic dermatitis (eczema) typically presents in childhood as a pruritic rash. This cohort study investigated whether there was an association between atopic dermatitis and other biological characteristics. The study population was children less than 6 years of age from general pediatric and family practices across Toronto, Canada who were followed longitudinally into their adolescence. From that, those with atopic dermatitis were selected based on a parental report (n = 2781) and their heights, weights, and BMI were analyzed compared to the WHO Child Growth Standards. Atopic dermatitis was associated with lower mean z-height (−0.13; 95% CI, −0.17 to −0.09; P < .001), higher mean z-BMI (0.05; 95% CI, 0.01 to 0.09; P = .008), and a lower mean z-weight (−0.07; 95% CI, −0.10 to −0.04;P < .001) compared with children without atopic dermatitis. Children with atopic dermatitis were, on average, approximately 0.5 cm shorter at age 2 years and 0.6 cm shorter at age 5 years than children without atopic dermatitis after adjusting for the covariates, although this did equalize around age 14. This is likely secondary to the effects on sleep, the steroids utilized for treatment, and chronic inflammation. Asthma was more common among children with atopic dermatitis, while there was no significant association with atopic dermatitis and diabetes and inflammatory bowel disease.
Main Takeaway: atopic dermatitis is associated with shorter stature, higher BMI, and lower weight, but the exact difference changes over time and becomes negligible as they age (14 years for height, 5.5 years for BMI), which is overall reassuring. Furthermore, the increased BMI in these children may be secondary to their shorter stature, hence there should be less concern for obesity in these children.
Main Takeaway: atopic dermatitis is associated with shorter stature, higher BMI, and lower weight, but the exact difference changes over time and becomes negligible as they age (14 years for height, 5.5 years for BMI), which is overall reassuring. Furthermore, the increased BMI in these children may be secondary to their shorter stature, hence there should be less concern for obesity in these children.
Vunakizumab significantly outperforms placebo treatment in moderate-to-severe plaque psoriasis
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Biologics are all the rage these days in the treatment of skin conditions…but let’s take a closer look before we jump to any rash conclusions. Psoriasis is a skin condition with a number of different subtypes, but is generally defined as an inflammatory skin condition that presents with scaly, erythematous plaques. In this double-blinded, randomized, phase II study, researchers administered varying doses of either vunakizumab, a new monoclonal antibody that targets IL-17A, or a placebo over a 36-week trial to 187 participants ≥ 18 years old with moderate-to-severe plaque psoriasis (defined as Psoriasis Area Severity Index [PASI] ≥ 12 and ≥ 10% body surface area [BSA] affected). The study’s primary outcome was the percentage of patients who achieved at least 75% improvement in PASI at 12 weeks. Taking place across 24 centers in multiple countries, the study randomly assigned participants to receive either vunakizumab at doses of 40, 80, 160, or 240 mg or placebo via subcutaneous injection for 36 weeks. At week 12, researchers found that the proportions of PASI 75 (75% skin clearance) responders in all vunakizumab groups (40, 80, 160, and 240 mg: 56.8%, 65.8%, 81.6%, and 86.5%, respectively; P < .001 vs placebo) were significantly higher than in the placebo group (5.4%) and showed significantly more skin clearance. They also found that the vunakizumab group showed dose-dependent improvements, with patients who received higher doses of medication experiencing a greater PASI response. Adverse events were reported in 108 out of 150 patients (72.0%) with vunakizumab treatment and 24 out of 37 patients (64.9%) who were given placebo treatment. The most common adverse events were injection site reaction, upper respiratory tract infections, and elevation of hepatic enzymes. Most adverse events were mild-to-moderate.
Main Takeaway: This study found that vunakizumab, a monoclonal antibody, significantly outperforms placebo treatment in the clearance of skin lesions in patients with moderate-to-severe plaque psoriasis, while demonstrating a similar safety profile. The proportion of patients who achieved PASI 75 at week 12 ranged from 56.8% to 86.5% with vunakizumab 40 mg to 240 mg, which showed significantly better results than the 5.4% placebo improvement. More studies are ultimately needed to study vunkizumab, but this trial showed promising efficacy and safety data, which is great news for patients who suffer from psoriasis.
Main Takeaway: This study found that vunakizumab, a monoclonal antibody, significantly outperforms placebo treatment in the clearance of skin lesions in patients with moderate-to-severe plaque psoriasis, while demonstrating a similar safety profile. The proportion of patients who achieved PASI 75 at week 12 ranged from 56.8% to 86.5% with vunakizumab 40 mg to 240 mg, which showed significantly better results than the 5.4% placebo improvement. More studies are ultimately needed to study vunkizumab, but this trial showed promising efficacy and safety data, which is great news for patients who suffer from psoriasis.
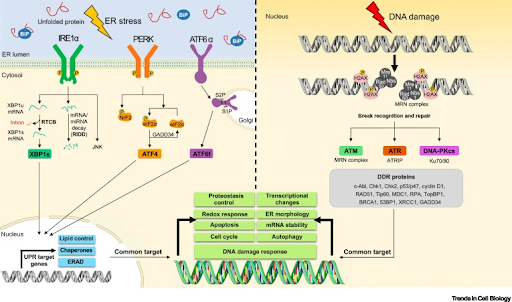
IRE1a affects the DNA damage response to UV radiation through calcium regulation
Journal of Investigative Dermatology
Journal of Investigative Dermatology
We know that too much sunlight can cause skin cancer. Part of this is because UV radiation, especially UVB radiation found in sunlight, directly damages DNA and initiates a DNA damage response. Recently, studies have linked the DNA damage response (DDR) with the unfolded protein response (UPR). The UPR helps relieve endoplasmic reticulum (ER) stress by getting rid of misfolded or unfolded proteins. One way cells try to decrease ER stress is through IRE1a, which degrades mRNAs or microRNAs through a process called IRE1a-dependent decay (RIDD). Currently, it is not known if RIDD plays a role in managing the DNA damage response related to UV radiation. In this study, the authors sought to better understand the role of IRE1a on cell stress and death.
First, they deleted IRE1a in keratinocytes of mice and found that this caused the skin to become more sensitive to UV radiation (they observed more apoptosis and sloughing). They reported that this is likely due to suppression of the UV DDR.
In neuronal cells, it is thought that IRE1a plays a role in calcium regulation. To see whether the DDR is linked to RIDD, they looked to the ER, which stores a lot of intracellular calcium. The authors found that loss of IRE1a also led to altered calcium levels in mouse skin keratinocytes through dysregulation of a specific ER calcium channel, Insp3R. In this study, the authors connected InsP3R, calcium regulation, and the UV DDR to IRE1a inactivation by UVB radiation.
Main Takeaway: Overall, this study supports a significant role of IRE1a in calcium regulation and DNA damage repair responses. Future studies are required to determine whether IRE1a can play a role in preventing forms of skin cancer.
First, they deleted IRE1a in keratinocytes of mice and found that this caused the skin to become more sensitive to UV radiation (they observed more apoptosis and sloughing). They reported that this is likely due to suppression of the UV DDR.
In neuronal cells, it is thought that IRE1a plays a role in calcium regulation. To see whether the DDR is linked to RIDD, they looked to the ER, which stores a lot of intracellular calcium. The authors found that loss of IRE1a also led to altered calcium levels in mouse skin keratinocytes through dysregulation of a specific ER calcium channel, Insp3R. In this study, the authors connected InsP3R, calcium regulation, and the UV DDR to IRE1a inactivation by UVB radiation.
Main Takeaway: Overall, this study supports a significant role of IRE1a in calcium regulation and DNA damage repair responses. Future studies are required to determine whether IRE1a can play a role in preventing forms of skin cancer.
QUESTION OF THE WEEK
NEJM CHALLENGE QUESTION
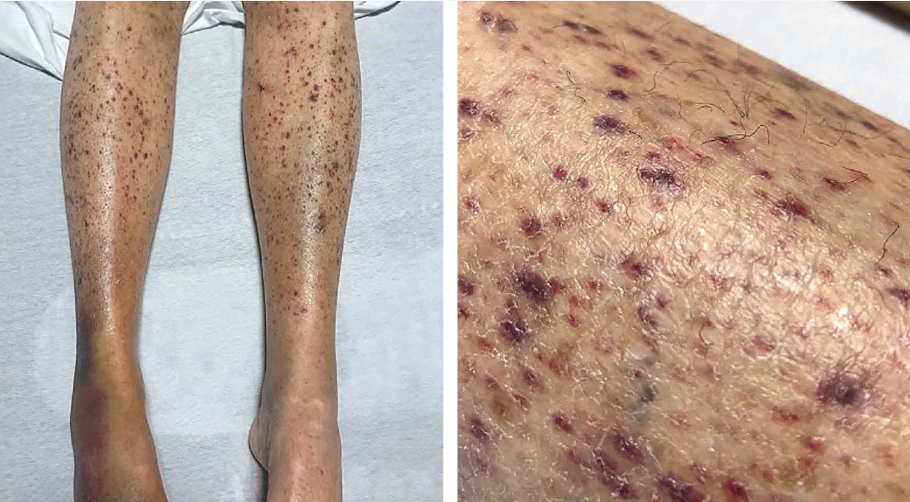
A 72-year-old woman with a history of esophageal strictures presented to the emergency department with a 3-month history of a rash on both legs. What is the most likely diagnosis?
1. Scurvy
2. Immune thrombocytopenic purpura
3. Covid-19 infection
4. Rocky mountain spotted fever
5. Granulomatosis with polyangiitis
1. Scurvy
2. Immune thrombocytopenic purpura
3. Covid-19 infection
4. Rocky mountain spotted fever
5. Granulomatosis with polyangiitis
Answer: Scurvy
The legs showed perifollicular petechiae, follicular hyperkeratosis, and corkscrew hairs. Examination of the oral mucosa showed gingival bleeding. The patient’s diet was limited due to esophageal stricture, and the measured plasma ascorbic acid level was less than 5 μmol per liter (0.1 mg per deciliter; reference range, 23 to 114 μmol per liter [0.4 to 2.0 mg per deciliter]).
Scurvy is due to vitamin C deficiency and typically presents with perifollicular purpura, “corkscrew hairs”, follicular hyperkeratosis, gingivitis, conjunctival hemorrhage, anemia, and difficulty walking. Major associations include fad diets, malnutrition (as in this case) and alcoholism.
Important fact: Vitamin C is a cofactor for lysyl hydroxylase and prolyl hydroxylase which are required for collagen hydroxylation and cross-linking. So, if you have vitamin C deficiency, you have defective collagen cross-linking which is why we see the skin findings as well as bone deformities, vascular fragility, and poor wound healing.
Other answers:
Immune thrombocytopenic purpura- this would present with manifestations of low platelets, including petechiae and gingival bleeding. However, you would not expect the corkscrew hairs and perifollicular purpura.
Covid-19 infection- this has a wide variety of cutaneous presentations, including morbilliform rash, pernio-like acral lesions, urticaria, macular erythema, vesicular eruption, papulosquamous eruption, and retiform purpura.
Rocky mountain spotted fever- this is due to infection with rickettsia rickettsii (#1 vector is dermacentor variabilis) and occurs 7-14 days post-tick bite with fever/headache/myalgias/GI symptoms and then 3-5 days later development of red macules on acral sites that spread centripetally to the trunk. Over time, these lesions become papular and petechial/purpuric due to edema and red blood cell extravasation from vessel destruction.
Granulomatosis with polyangiitis- this is an ANCA + vasculitis which presents with nasal symptoms (sinusitis, rhinorrhea), pulmonary (cough, hemoptysis), renal (glomerulonephritis with hematuria) and CNS (peripheral neuropathy, CVA). Cutaneous lesions include palpable purpura, pyogenic granuloma like nodules, and strawberry gums.
The legs showed perifollicular petechiae, follicular hyperkeratosis, and corkscrew hairs. Examination of the oral mucosa showed gingival bleeding. The patient’s diet was limited due to esophageal stricture, and the measured plasma ascorbic acid level was less than 5 μmol per liter (0.1 mg per deciliter; reference range, 23 to 114 μmol per liter [0.4 to 2.0 mg per deciliter]).
Scurvy is due to vitamin C deficiency and typically presents with perifollicular purpura, “corkscrew hairs”, follicular hyperkeratosis, gingivitis, conjunctival hemorrhage, anemia, and difficulty walking. Major associations include fad diets, malnutrition (as in this case) and alcoholism.
Important fact: Vitamin C is a cofactor for lysyl hydroxylase and prolyl hydroxylase which are required for collagen hydroxylation and cross-linking. So, if you have vitamin C deficiency, you have defective collagen cross-linking which is why we see the skin findings as well as bone deformities, vascular fragility, and poor wound healing.
Other answers:
Immune thrombocytopenic purpura- this would present with manifestations of low platelets, including petechiae and gingival bleeding. However, you would not expect the corkscrew hairs and perifollicular purpura.
Covid-19 infection- this has a wide variety of cutaneous presentations, including morbilliform rash, pernio-like acral lesions, urticaria, macular erythema, vesicular eruption, papulosquamous eruption, and retiform purpura.
Rocky mountain spotted fever- this is due to infection with rickettsia rickettsii (#1 vector is dermacentor variabilis) and occurs 7-14 days post-tick bite with fever/headache/myalgias/GI symptoms and then 3-5 days later development of red macules on acral sites that spread centripetally to the trunk. Over time, these lesions become papular and petechial/purpuric due to edema and red blood cell extravasation from vessel destruction.
Granulomatosis with polyangiitis- this is an ANCA + vasculitis which presents with nasal symptoms (sinusitis, rhinorrhea), pulmonary (cough, hemoptysis), renal (glomerulonephritis with hematuria) and CNS (peripheral neuropathy, CVA). Cutaneous lesions include palpable purpura, pyogenic granuloma like nodules, and strawberry gums.
sk(in depth) recap
1. In Chien et al., they identified ____ as a potential mediator of retinoid efficacy in reducing symptoms of photoaging.
A. MMP1
B. MMP2
C. MMP3
D. MMP9
2. According to findings from Gupta et al., how should you manage patients with BWH T2a-high tumors?
A. Close clinical surveillance and consider radiologic imaging
B. Close clinical surveillance but do not consider radiologic imaging
C. As needed follow-up
3. What are proposed mechanisms for the female-sex bias in autoimmune disorders?
A. Physiologic differences in immune cell composition and function
B. Sex hormones
C. X chromosome inactivation
D. Genetics
E. All of the above
A. MMP1
B. MMP2
C. MMP3
D. MMP9
2. According to findings from Gupta et al., how should you manage patients with BWH T2a-high tumors?
A. Close clinical surveillance and consider radiologic imaging
B. Close clinical surveillance but do not consider radiologic imaging
C. As needed follow-up
3. What are proposed mechanisms for the female-sex bias in autoimmune disorders?
A. Physiologic differences in immune cell composition and function
B. Sex hormones
C. X chromosome inactivation
D. Genetics
E. All of the above
- In Chien et al., they identified ____ as a potential mediator of retinoid efficacy in reducing symptoms of photoaging.
B. MMP2
C. MMP3
D. MMP9
Although matrix metalloproteinases have long been thought to be involved in the mechanistic action of retinoids, the authors found that there was not a significant difference in MMP1, MMP3, MMP9, or procollagen I expression. Instead, the authors identified a significant reduction in MMP2 (a metalloproteinase involved in type IV collagen degradation) expression.
2. According to findings from Gupta et al., how should you manage patients with BWH T2a-high tumors?
A. Close clinical surveillance and consider radiologic imaging
B. Close clinical surveillance but do not consider radiologic imaging
C. As needed follow-up
BWH T2a-high tumors carry an 8% risk of developing poor outcomes, such as metastasis or death, which is 3x higher than the risk of BWH T2a-low tumors. The authors found that 69% of these poor outcomes were detectable with imaging but not necessarily with clinical examination alone. Thus, the authors recommend close surveillance with consideration of additional radiologic surveillance.
3. What are proposed mechanisms for the female-sex bias in autoimmune disorders?
A. Physiologic differences in immune cell composition and function
B. Sex hormones
C. X chromosome inactivation
D. Genetics
E. All of the above
In this review by Xing et al., the authors discuss all of the above as potential players in the female sex-bias in autoimmune disorders, such as lupus, Sjogren’s and systemic sclerosis. Future studies are necessary to identify additional contributing factors to the development of autoimmune disorders.