FIFTEENTH ISSUE
July 27th, 2022
Sk(in depth) scoop
Cooler Heads: the newest FDA cleared scalp cooling device for chemotherapy-induced alopecia
There’s some hot news for cooler heads. In December, 2021 technology startup Cooler Heads gained FDA clearance for its scalp cooling system, Amma™, becoming the first portable cold cap available in the United States.
Scalp cooling systems were first introduced in the 1970s in Europe as a means of preventing chemotherapy-induced alopecia, frequently cited as one of the most distressing consequences of chemotherapy for patients.¹ Scalp cooling is believed to be both safe and effective, with some studies suggesting that more than 50% of patients can maintain more than half of their hair after using the technology!² Although scalp cooling systems have existed for decades, it wasn’t until 2015 that the FDA cleared a scalp cooling system for patient use.³
So what sets Amma™ apart?
· The system is transportable, allowing patients to limit the amount of time they spend at an infusion center
· Patients can rent the portable scalp cooling machine and take it home with them
· Amma’s parent company, Cooler Heads, was founded by a breast cancer survivor who herself benefited from scalp cooling technology
Main takeaway: Though chemotherapy-induced alopecia remains one of the most distressing consequences of chemotherapy, there are an increasing number of devices available to mitigate its impact. The FDA clearance of Amma™ as a scalp cooling system represents another victory for cancer survivors in the United States, who will be able to receive life-saving treatment while maintaining their hair and sense of self.
1. Freites-Martinez A, Shapiro J, Goldfarb S, et al. Hair disorders in patients with cancer. J Am Acad Dermatol. 2019. doi:10.1016/j.jaad.2018.03.055
2. Nangia J, Wang T, Osborne C, et al. Effect of a Scalp Cooling Device on Alopecia in Women Undergoing Chemotherapy for Breast Cancer: The SCALP Randomized Clinical Trial. JAMA. 2017;317(6):596-605. doi:10.1001/jama.2016.20939
3. Novice T, Novice M, Shapiro J, Lo Sicco K. Chemotherapy-induced alopecia-A potentially preventable side effect with scalp cooling. J Am Acad Dermatol. 2020;82(2):e57-e59. doi:10.1016/j.jaad.2019.09.059
Is Berdazimer gel 10.3% effective for treating molluscum contagiosum?
JAMA Dermatology
JAMA Dermatology
Where is Harry when you need him to ward off the molluscum?! Molluscum contagiosum (MC) is a common, and highly contagious, skin condition. It usually presents in children between the ages of 1-14. Clinically, the papules are pink, round, and often 1-6mm in size with central umbilication. Patients may be infected for months to years and may range from having few to hundreds of lesions at a given time. Treatment options have been limited. Ablation, cryotherapy or chemical destruction are available procedural options, but unfortunately repeat visits are typically required and such treatments may be painful.
Nitric oxide has been shown to play roles in immunomodulation, cytokine production, and inflammatory, NF-kB and apoptosis pathways. Berdazimer gel 10.3% is a novel topical nitric oxide-releasing agent. It is composed of a berdazimer sodium gel and hydrogel proton donor, which uniquely allows nitric oxide to be released at the targeted skin surface. It is hypothesized that this novel topical therapy can treat molluscum contagiosum.
A randomized Phase 3 clinical trial investigated berdazimer gel’s efficacy in the treatment of MC. This study included 891 participants from 55 participating cites. Patients were 6 months of age or older and were randomized into treatment (n=444) and control (n=447) groups. They applied gel to all lesions daily for 12 weeks. At the end of the study, significant improvements were found in the treatment group; 32.4% (n=144) of patients treated with topical berdazimer gel (10.3%) showed complete clearance of MC by end of the trial, compared to 19.7% in the control group (absolute difference 12.7; odds ratio 2.0; 95% CI 1.5-2.8, p < 0.001).
This study was limited in that sufficient evaluation by age, race and ethnicity were not performed. Additionally, analyses into the therapeutic potential for patients with sexually transmitted MC were not performed.
Main Takeaway: Berdazimer gel 10.3% significantly improved clearance rates in patients with MC after 12 weeks of use.
CTP-543, a JAK inhibitor, significantly reduces hair loss in alopecia areata
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
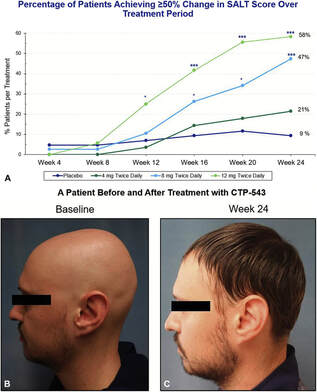
Attention: high yield news ahead for those suffering from alopecia! Alopecia areata (AA) is an autoimmune condition that causes nonscarring, smooth patches of hair loss. AA affects 0.2% of the population and can have severe psychological impact on patients. AA pathophysiology involves cytokines, including IFN-γ and IL-15 via the Janus Kinase (JAK) signal transducer pathway. JAK inhibition could play a role in the treatment of AA. In this Phase 2, double blind, randomized trial, researchers tested the safety and efficacy of CTP-543, a selective JAK1 and JAK2 inhibitor. 149 patients between ages 18 and 65 with active AA and ≥50% hair loss (as defined by the Severity of Alopecia Tool [SALT]) were divided into 3 cohorts. Each cohort received either 4, 8, or 12 mg of CTP-543 twice daily for 24 weeks, with each cohort randomized to either placebo or control.
The primary outcome of this study was the proportion of subjects achieving ≥50% relative reduction in SALT scores from baseline. Results showed a statistically significant dose-dependent (p<0.05) reduction in SALT scores from baseline for the 8 and 12 mg cohorts versus placebo. Patients’ self-reported assessment of “much improved” after 24 weeks was also statistically significant versus placebo (p<0.001) for the 8 and 12 mg cohorts. CTP-543 was well-tolerated, and most adverse effects were rated as mild or moderate.
Main takeaway: Researchers found that CTP-453, a JAK inhibitor, significantly reduced severity of hair loss in AA from baseline after 24 weeks, with dose-dependent increases in response.
Stratum corneum ceramide profiles provide reliable indicators of remission and potential flares in atopic dermatitis
Journal of Investigative Dermatology
Journal of Investigative Dermatology
Scratching the atopic dermatitis itch. Atopic dermatitis is thought of as a chronic, itchy, inflammatory skin condition. Proposed mechanisms include 1) impairment of skin barrier function and 2) deficits in its ability to hold onto water. Patients with atopic dermatitis may have periods of remission and exacerbation despite regular topical steroid and daily moisturizer use.
Both filaggrin (FLG) and ceramides found within the stratum corneum are thought to play important roles in skin barrier function. Therefore, the authors hypothesized that mutations in filaggrin or differences in the stratum corneum ceramide profiles affect remission and exacerbation of atopic dermatitis.
They examined two groups of patients: those in remission without subsequent exacerbation at 8 weeks and those with subsequent exacerbation at 8 weeks. They examined 11 loss of function filaggrin mutations and found that exacerbation of atopic dermatitis was not associated with specific filaggrin mutations.
Analysis of the stratum corneum ceramide profiles during the remission phase identified differences between the study groups that predicted subsequent exacerbations of atopic dermatitis. Specifically, they found that the carbon chain lengths of specific ceramides (NDS, NS, NH, and AH) were shorter in patients who had subsequent atopic dermatitis exacerbation compared to those who did not.
Limitations of the study include geographical restriction to Japan and clinically defined measures for “remission.” Future studies are required to see whether ceramides may play a role in atopic dermatitis pathogenesis or whether they may serve as clinical biomarkers for atopic dermatitis exacerbations.
Main takeaway and limitations: Ceramide profiles of the stratum corneum may help predict remission and/or exacerbation of atopic dermatitis.
Both filaggrin (FLG) and ceramides found within the stratum corneum are thought to play important roles in skin barrier function. Therefore, the authors hypothesized that mutations in filaggrin or differences in the stratum corneum ceramide profiles affect remission and exacerbation of atopic dermatitis.
They examined two groups of patients: those in remission without subsequent exacerbation at 8 weeks and those with subsequent exacerbation at 8 weeks. They examined 11 loss of function filaggrin mutations and found that exacerbation of atopic dermatitis was not associated with specific filaggrin mutations.
Analysis of the stratum corneum ceramide profiles during the remission phase identified differences between the study groups that predicted subsequent exacerbations of atopic dermatitis. Specifically, they found that the carbon chain lengths of specific ceramides (NDS, NS, NH, and AH) were shorter in patients who had subsequent atopic dermatitis exacerbation compared to those who did not.
Limitations of the study include geographical restriction to Japan and clinically defined measures for “remission.” Future studies are required to see whether ceramides may play a role in atopic dermatitis pathogenesis or whether they may serve as clinical biomarkers for atopic dermatitis exacerbations.
Main takeaway and limitations: Ceramide profiles of the stratum corneum may help predict remission and/or exacerbation of atopic dermatitis.
Patients are Willing and Successful with Home Suture Removal after Mohs Surgical Procedures
Dermatologic Surgery
Dermatologic Surgery
DIY comes to dermatology. Mohs surgery is a microscopically controlled surgery used to treat both common and rare types of skin cancer. Typically, patients will return to Mohs Surgery clinics for post-operative suture removal. However, this study investigated whether patients were both willing and able to successfully remove sutures at home after having Mohs surgery.
150 patients were screened on their willingness to participate with 90.1% being willing to attempt self-removal. Women reported 98% willingness to attempt compared to men at 86.7% (p=0.035). Those who were willing were provided two resources to aid them in completion of at-home removal: one handout with photos and instructions and one video. Of the 133 patients who followed up after the procedure (3 were lost to follow up), 97% successfully removed the sutures at home. Of the four who did not, two attempted but were unable to complete removal due to difficulty and two did not end up attempting. These four patients’ sutures were all removed in the clinic. The Mohs Micrographic Surgery population is often older than 60 years old, and commute time was significantly reduced for patients. In this study, returning to the clinic for suture removal would have required 34% of patients to drive at least 30 minutes and 12% to drive over an hour.
Main takeaway: This study demonstrated that the large majority of Mohs Surgery patients were willing and successful with at-home suture removal.