SIXTEENTH ISSUE
August 10th, 2022
What a plant-tastic idea!
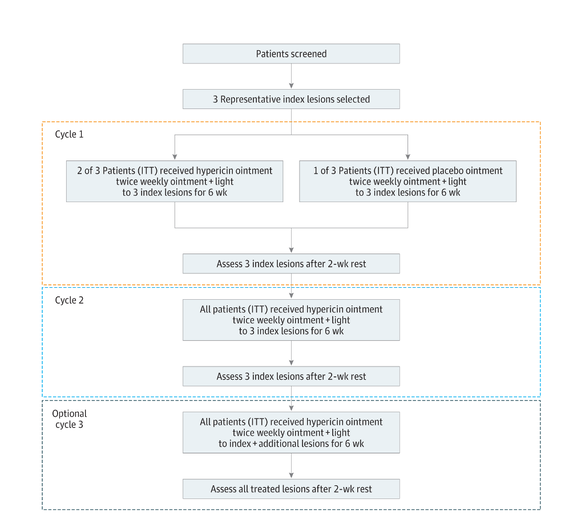
Mycosis fungoides−cutaneous T-cell lymphoma (MF/CTCL) is a cutaneous lymphoma composed mostly of malignant T-cells. While primarily treated with topical agents in the early stages of disease, these treatments are highly toxic. Hypericin is a plant-derived, light-activated drug that inhibits T-cell proliferation as it has a predilection for malignant cells and induces apoptosis. When used systemically, it has been associated with intense phototoxicity. As a potential alternative treatment, a synthetic hypericin ointment (HyBryte) was created as a topical photodynamic therapy (PDT). It was evaluated in this phase 3, placebo-controlled, double-blind, multicenter randomized clinical trial.
Mycosis fungoides−cutaneous T-cell lymphoma (MF/CTCL) is a cutaneous lymphoma composed mostly of malignant T-cells. While primarily treated with topical agents in the early stages of disease, these treatments are highly toxic. Hypericin is a plant-derived, light-activated drug that inhibits T-cell proliferation as it has a predilection for malignant cells and induces apoptosis. When used systemically, it has been associated with intense phototoxicity. As a potential alternative treatment, a synthetic hypericin ointment (HyBryte) was created as a topical photodynamic therapy (PDT). It was evaluated in this phase 3, placebo-controlled, double-blind, multicenter randomized clinical trial.
The hypericin PDT-treated group had a statistically significant index lesion response rate (ILRR) of 16% (19 of 116 patients) compared with 4% in the placebo-treated group (2 of 50 patients; P = .04). Analysis of all patients who received hypericin PDT demonstrated a consistent ILRR of 18% after 6 weeks of treatment and 40% after 12 weeks. Consolidated response rates across all individual index lesions were similar in both patch and plaque lesions suggesting adequate penetration into lesions. The adverse events were similar in both treatment groups during cycle 1 with the exception of slightly more treatment-site reactions with hypericin PDT.
Limitations include a short duration of treatment for each cycle and lack of correlation between treatment response and varying amounts of skin pigmentation.
Main Takeaway: Topical hypericin PDT is an effective and safe alternative to prior topical or systemic treatments for early-stage MF/CTCL.
Limitations include a short duration of treatment for each cycle and lack of correlation between treatment response and varying amounts of skin pigmentation.
Main Takeaway: Topical hypericin PDT is an effective and safe alternative to prior topical or systemic treatments for early-stage MF/CTCL.
Increasing Breslow thickness has decreased correlation with survival in ultrathick melanomas
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Why thick doesn’t always mean bad!
Breslow thickness is an important prognostic indicator of melanoma metastasis, recurrence, and survival. It is measured in millimeters from the granular layer of the epidermis to the deepest layer of involvement. “Ultrathick” melanomas (defined as ≥15 mm) are uncommon and little is known about how well Breslow thickness determines prognosis for these tumors. In this retrospective cohort study of 5595 patients with cutaneous melanomas of Breslow thickness ≥4 mm, researchers compared the overall survival (OS) and recurrence-free survival (RFS) of patients with thick (4-8 mm Breslow thickness) melanomas versus ultrathick (≥15 mm Breslow thickness) melanomas.
Patients from the Dutch Pathology Registry with melanomas diagnosed between 2000 and 2014 were stratified into 4 Breslow thickness groups: 4-10 mm, 10-15 mm, 15-20 mm, and >20 mm. These cohorts were analyzed and compared to each other, with the primary outcome being differences in OS and RFS (p<0.05). The 5-year OS rates for patients with melanomas of 4-10 mm, 10-15 mm, 15-20 mm, and >20 mm were 52.9% (95% CI, 51.4-54.4), 35.9% (95% CI, 31.2-41.3), 34.5% (95% CI, 25.9-46.0), and 47.9% (95% CI, 37.3-61.6), respectively. The 5-year RFS rates reflected similar trends. Limitations include a small sample size for melanomas 15-20 mm and >20 mm.
Main takeaway: This study found that increasing Breslow thickness in ultrathick melanomas (>15 mm) has decreased correlation with survival outcomes than previously thought.
Neutrophil Extracellular Traps in Hidradenitis Suppurativa may be due anti-DNase antibodies
Journal of Investigative Dermatology
Journal of Investigative Dermatology
Never ever spell part backwards. It's a trap!
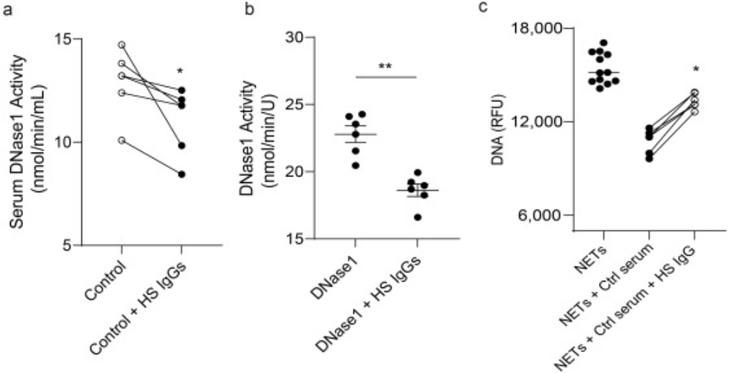
Hidradenitis suppurativa (HS) is an inflammatory disorder characterized by painful skin nodules, fistulas, and scarring. In prior reports, HS has been linked to inflammatory findings such as neutrophil extracellular trap (NET) infiltration in skin lesions and the presence of autoantibodies. NETs can activate harmful immune responses (which has been seen in other autoimmune and inflammatory diseases), and removal of NETs can help prevent inflammatory damage to tissues. The authors hypothesized that the NETs present in HS patients exist because they are trapped and not effectively cleared by DNases, like 1 and 1L3.
The study found that over 90% of HS patients do not degrade NETs. In a subset of HS patients, adding extra DNase to serum from HS patients restored NET degradation. In particular, they also found increased levels of anti-DNase 1 and anti-DNase 1L3 antibodies in HS serum and skin lesions, and more severe disease correlated with increased levels of these antibodies. Finally, the authors demonstrated that neutralizing Anti-DNase 1 antibodies from HS patients impair DNase activity and NET breakdown (see figure).
Limitations of this study include a relatively small cohort of primarily African American race.
Hidradenitis suppurativa (HS) is an inflammatory disorder characterized by painful skin nodules, fistulas, and scarring. In prior reports, HS has been linked to inflammatory findings such as neutrophil extracellular trap (NET) infiltration in skin lesions and the presence of autoantibodies. NETs can activate harmful immune responses (which has been seen in other autoimmune and inflammatory diseases), and removal of NETs can help prevent inflammatory damage to tissues. The authors hypothesized that the NETs present in HS patients exist because they are trapped and not effectively cleared by DNases, like 1 and 1L3.
The study found that over 90% of HS patients do not degrade NETs. In a subset of HS patients, adding extra DNase to serum from HS patients restored NET degradation. In particular, they also found increased levels of anti-DNase 1 and anti-DNase 1L3 antibodies in HS serum and skin lesions, and more severe disease correlated with increased levels of these antibodies. Finally, the authors demonstrated that neutralizing Anti-DNase 1 antibodies from HS patients impair DNase activity and NET breakdown (see figure).
Limitations of this study include a relatively small cohort of primarily African American race.
Figure. IgG antibodies from HS patients impair DNase activity.
Main takeaway: There are anti-DNase 1 and anti-DNase 1L3 antibodies in patients with HS that prevent effective breakdown of NETs, which may contribute to disease. Perhaps, DNase 1 activity could be targeted in future therapies for HS.
Facial hyperhidrosis: examining Botox or 2% glycopyrrolate as a preferred treatment option
Dermatologic Surgery
Dermatologic Surgery
Two great options for too much sweat! Facial hyperhidrosis, or excessive sweating, affects patients both cosmetically and psychologically. This study compared glycopyrrolate to Botox in treatment of facial hyperhidrosis.
Utilizing the starch iodine test to measure sweat output, 24 patients were sorted randomly into two equal groups, with one receiving Botox and one receiving 2% glycopyrrolate. Nine of the twelve patients (75%) in the Botox group achieved complete response, and nine of the twelve patients (75%) in the glycopyrrolate group also achieved complete response. In both groups, the Hyperhidrosis Disease Severity (HDSS) and Dermatology Life Quality Index (DLQI) scores were improved. The groups differed in treatment response time and duration: the glycopyrrolate group had a quicker, but shorter benefit.
While the results demonstrated an adequate response to both treatments, only 24 patients were utilized in the study.
Main Takeaway: Both Botox and 2% glycopyrrolate showed statistical significance in the treatment of facial hyperhidrosis. The glycopyrrolate group had a faster onset with a shorter overall duration compared to the Botox group.
Utilizing the starch iodine test to measure sweat output, 24 patients were sorted randomly into two equal groups, with one receiving Botox and one receiving 2% glycopyrrolate. Nine of the twelve patients (75%) in the Botox group achieved complete response, and nine of the twelve patients (75%) in the glycopyrrolate group also achieved complete response. In both groups, the Hyperhidrosis Disease Severity (HDSS) and Dermatology Life Quality Index (DLQI) scores were improved. The groups differed in treatment response time and duration: the glycopyrrolate group had a quicker, but shorter benefit.
While the results demonstrated an adequate response to both treatments, only 24 patients were utilized in the study.
Main Takeaway: Both Botox and 2% glycopyrrolate showed statistical significance in the treatment of facial hyperhidrosis. The glycopyrrolate group had a faster onset with a shorter overall duration compared to the Botox group.