THIRTY-sixth ISSUE
june 14, 2023
How does plasmapheresis compare to IVIG as the first treatment after failed corticosteroid therapy for SJS/TEN?
JAMA Dermatology
So the steroids didn’t work…now what?
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are severe adverse cutaneous reactions to medication or infection. Initially presenting as flu-like symptoms, a sloughing rash eventually develops across skin and mucous membranes. SJS/TEN is difficult to treat; complications include sepsis, multi-organ failure, and death with a mortality rate of 10% and 30% for SJS/TEN respectively.
Researchers were curious if patients who failed corticosteroids showed better outcomes if the second treatment was plasmapheresis versus IVIG. This 9-year retrospective cohort study in Japan (n=266) measured in-hospital mortality, length of hospital stay, and overall medical costs.
What did they find?
Limitations: Results may be confounded as some patients who initially underwent plasmapheresis were subsequently treated with IVIG. Additionally, generalizability is limited as analysis was limited to Japanese hospitals.
Main Takeaway: No significant differences in mortality were seen when initiating plasmapheresis vs. IVIG therapy in SJS/TEN patients who failed corticosteroids; plasmapheresis may be associated with longer hospital stays and overall higher medical costs.
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are severe adverse cutaneous reactions to medication or infection. Initially presenting as flu-like symptoms, a sloughing rash eventually develops across skin and mucous membranes. SJS/TEN is difficult to treat; complications include sepsis, multi-organ failure, and death with a mortality rate of 10% and 30% for SJS/TEN respectively.
Researchers were curious if patients who failed corticosteroids showed better outcomes if the second treatment was plasmapheresis versus IVIG. This 9-year retrospective cohort study in Japan (n=266) measured in-hospital mortality, length of hospital stay, and overall medical costs.
What did they find?
- Plasmapheresis was used first after steroids for 53 patients, while IVIG was used first after steroids for 213 patients
- No significant difference in mortality rate was observed between groups (18.3% vs 19.5%; OR, 0.93; 95% CI, 0.38–2.23; P = .86)
- The plasmapheresis group had an overall longer hospital stay (45.3 vs 32.8 days; difference,12.5 days; 95% CI, 0.4–24.5 days; P = .04)
- The plasmapheresis group incurred higher overall medical costs (US $34,262 vs $23,054; difference, $11,207; 95% CI, $2,789–$19,626; P = .009)
Limitations: Results may be confounded as some patients who initially underwent plasmapheresis were subsequently treated with IVIG. Additionally, generalizability is limited as analysis was limited to Japanese hospitals.
Main Takeaway: No significant differences in mortality were seen when initiating plasmapheresis vs. IVIG therapy in SJS/TEN patients who failed corticosteroids; plasmapheresis may be associated with longer hospital stays and overall higher medical costs.
Paroxetine is an effective treatment for refractory erythema of rosacea: primary results from a RCT
JAAD
Paroxetine packs a punch to rosacea!
Rosacea is a chronic inflammatory condition that causes facial erythema, telangiectasias, and papules/pustules. While oral doxycycline, topical brimonidine (α2-adrenergic receptor agonist), and topical oxymetazoline ( α1A adrenoceptor agonist) are current treatment options, there are cases refractory to these medications.
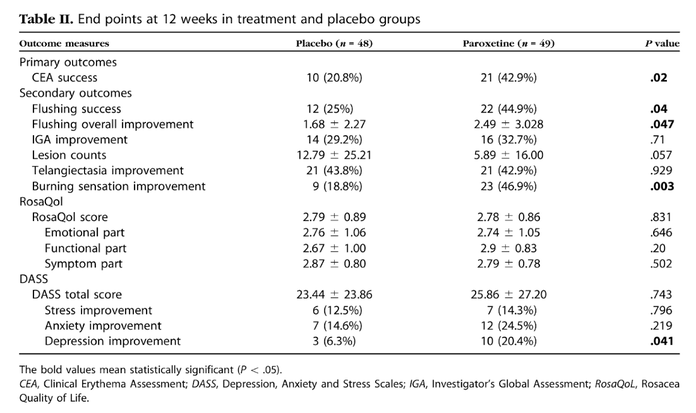
The goal of this multicenter, prospective, randomized, double-blinded, placebo-controlled trial (n=97) was to evaluate the efficacy of paroxetine for treatment of refractory erythema of rosacea. Subjects received 25 mg of paroxetine daily for 12 weeks; placebo was given to control subjects. Post-trial Clinical Erythema Assessments (CEA) were used to evaluate changes from baseline.
What did they find?
· The paroxetine group demonstrated significant improvement in erythema compared to controls (42.9% vs. 20.8% improvement, P = 0.02)
· The paroxetine group reported an improvement in overall flushing compared to controls (2.49 ± 3.028 vs 1.68 ± 2.27, P = 0.047)
· Burning sensation improved ≥2 points from baseline more frequently in the paroxetine treatment group (46.9% vs. 18.8%, P=0.003)
Limitations: The trial used a single-dose regimen of paroxetine (25 mg); future studies should explore different dosages. Additionally, the follow-up period was relatively short, thus limiting ability to assess long-term efficacy of paroxetine.
Main Takeaway: Paroxetine may be an effective treatment option for treating rosacea-induced erythema, flushing, and burning.
Rosacea is a chronic inflammatory condition that causes facial erythema, telangiectasias, and papules/pustules. While oral doxycycline, topical brimonidine (α2-adrenergic receptor agonist), and topical oxymetazoline ( α1A adrenoceptor agonist) are current treatment options, there are cases refractory to these medications.
The goal of this multicenter, prospective, randomized, double-blinded, placebo-controlled trial (n=97) was to evaluate the efficacy of paroxetine for treatment of refractory erythema of rosacea. Subjects received 25 mg of paroxetine daily for 12 weeks; placebo was given to control subjects. Post-trial Clinical Erythema Assessments (CEA) were used to evaluate changes from baseline.
What did they find?
· The paroxetine group demonstrated significant improvement in erythema compared to controls (42.9% vs. 20.8% improvement, P = 0.02)
· The paroxetine group reported an improvement in overall flushing compared to controls (2.49 ± 3.028 vs 1.68 ± 2.27, P = 0.047)
· Burning sensation improved ≥2 points from baseline more frequently in the paroxetine treatment group (46.9% vs. 18.8%, P=0.003)
Limitations: The trial used a single-dose regimen of paroxetine (25 mg); future studies should explore different dosages. Additionally, the follow-up period was relatively short, thus limiting ability to assess long-term efficacy of paroxetine.
Main Takeaway: Paroxetine may be an effective treatment option for treating rosacea-induced erythema, flushing, and burning.
Lichen sclerosus… a chronic condition ‘lichen’ no other
Vulvar lichen sclerosus (VLS) is an inflammatory condition characterized by atrophic, tender/pruritic patches. VLS can profoundly affect patients’ self-image and quality of life. This qualitative interview study sought to better understand the patient perspective of those living with VLS. Virtual interviews or phone calls were conducted with 20 patients living with VLS who were identified from online support groups or social media.
What did they find?
Limitations: This qualitative study was based on semi-structured patient interviews; additional controlled studies would be helpful in better understanding these important themes in VLS. Generalizability of this study may be limited as the study involved 20 participants identified through social media or online support groups who primarily self-identified as White.
Main Takeaway: Further efforts are needed to provide better care for patients with VLS, ranging from helping patients feel heard and correctly diagnosing VLS, to educating patients on self-management and providing community support.
Vulvar lichen sclerosus (VLS) is an inflammatory condition characterized by atrophic, tender/pruritic patches. VLS can profoundly affect patients’ self-image and quality of life. This qualitative interview study sought to better understand the patient perspective of those living with VLS. Virtual interviews or phone calls were conducted with 20 patients living with VLS who were identified from online support groups or social media.
What did they find?
- Three major themes from patient interviews included:
- Missed opportunities, which refers to delayed or missed diagnosis, lack of information, unsatisfying interactions within healthcare
- Learning to live with a chronic condition, which includes the patient work involved in learning to care for VLS and its impact on everyday life
- Living a secret life, which refers to how VLS is an isolating and often hidden disease, and how there remains a stigma with diseases affecting the anogenital region
Limitations: This qualitative study was based on semi-structured patient interviews; additional controlled studies would be helpful in better understanding these important themes in VLS. Generalizability of this study may be limited as the study involved 20 participants identified through social media or online support groups who primarily self-identified as White.
Main Takeaway: Further efforts are needed to provide better care for patients with VLS, ranging from helping patients feel heard and correctly diagnosing VLS, to educating patients on self-management and providing community support.
Pediatric oncology patients on anti-cancer therapy are more likely to have more numerous and persistent warts
Pediatric Dermatology
Should we be worrywarts about warts on pediatric oncology patients?
Warts are common, benign, epidermal lesions caused by human papillomavirus (HPV). While generally self-limited, warts may have increased prevalence and longer duration in immunocompromised children. This 10-year retrospective study evaluated the characteristics and outcomes of cutaneous warts in pediatric oncology patients, 37.3% of whom were on active oncology treatment and 62.7% of whom were not on active oncology treatment.
What did they find?
Main Takeaways: This study highlighted the challenges of treating warts in pediatric oncology patients receiving active anti-cancer treatment, who are more likely to have persistent or worsening warts with treatment compared to patients not on anti-cancer treatment.
Warts are common, benign, epidermal lesions caused by human papillomavirus (HPV). While generally self-limited, warts may have increased prevalence and longer duration in immunocompromised children. This 10-year retrospective study evaluated the characteristics and outcomes of cutaneous warts in pediatric oncology patients, 37.3% of whom were on active oncology treatment and 62.7% of whom were not on active oncology treatment.
What did they find?
- 72 patients with hematologic malignancies (55.1%), CNS tumors (15.4%), neuroblastoma (11.5%), bone tumors (7.7%), and melanoma (1.3%) were enrolled
- Anti-cancer treatment regimens included cytotoxic chemotherapy (80.8%) and targeted therapies including immunotherapy (23.0%)
- Plantar warts were most common (53.8%)
- 60.3% of patients had >5 warts at the time of presentation
- Wart treatment regimens included cryotherapy (n=59) and topical salicylic acid (n=50)
- 56.0% of patients actively receiving oncology treatment had persistent or worsened warts with treatment, compared to 13.4% of patients not on active oncology treatment
- Only 24.0% of patients on active anti-cancer treatment had complete resolution of warts with treatment, compared to 63.3% of patients not on active oncology treatment
Main Takeaways: This study highlighted the challenges of treating warts in pediatric oncology patients receiving active anti-cancer treatment, who are more likely to have persistent or worsening warts with treatment compared to patients not on anti-cancer treatment.
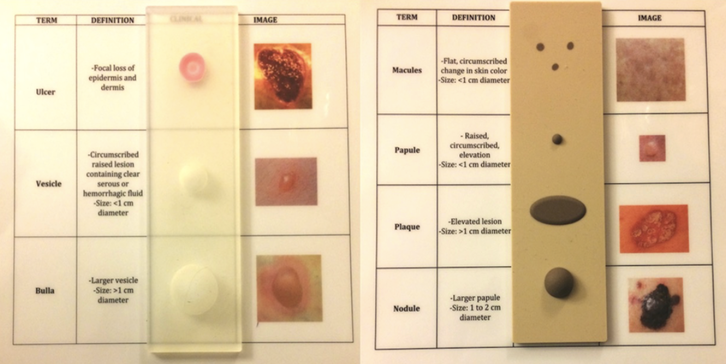
Are we changing the way we teach medical students dermatology with a 3D skin lesion model?
Journal of the American Academy of Dermatology
Medical education you can ~feel~
Medical education lacks basic dermatologic identification and training despite the fact that non-dermatologists are typically the first to lay eyes on most skin lesions. To better educate medical students and emphasize the importance of skin cancer examination, a 3D printed, silicone tactile learning tool (TLT) was created.
First-year medical students at the University of Colorado piloted the use of the TLT in a pre-clerkship dermatology course; their satisfaction with the tool, confidence in identifying the lesions, importance of and overall usefulness of the TLT in understanding skin lesions was evaluated.
What did they find?
Main takeaway: Utilizing TLT in a first year medical education dermatology course may enhance student confidence in determining and understanding skin lesions.
Medical education lacks basic dermatologic identification and training despite the fact that non-dermatologists are typically the first to lay eyes on most skin lesions. To better educate medical students and emphasize the importance of skin cancer examination, a 3D printed, silicone tactile learning tool (TLT) was created.
First-year medical students at the University of Colorado piloted the use of the TLT in a pre-clerkship dermatology course; their satisfaction with the tool, confidence in identifying the lesions, importance of and overall usefulness of the TLT in understanding skin lesions was evaluated.
What did they find?
- 184 students participated in the preclerkship course with 52% responding to the TLT-specific survey using a 5 point Likert-Scale with 5 being most favorable
- The mean scores for the recorded survey questions were found to be:
- 4.49 (SD 0.75) was determined for the use of TLT to help describe skin lesions
- 4.25 (SD 0.76) for its ability to improve confidence in describing skin lesions
- 4.20 (SD 0.83) on their opinion of importance of TLT in the use of first year medical school education
- 4.34 (SD 0.68) on if TLT helped solidify their knowledge of skin lesions
Main takeaway: Utilizing TLT in a first year medical education dermatology course may enhance student confidence in determining and understanding skin lesions.