eigth issue
April 20th, 2022
Improvement in psoriasis for the kiddos with Ixekizumab
JAMA Dermatology
Don’t forget about the kiddos! Psoriasis affects about 1% of children and can have significant effects on their quality of life, as well as multiple comorbidities. Ixekizumab is approved as a first-line option for treatment of moderate to severe psoriasis in children ages 6-18 years old. Prior studies had shown this to be superior to placebo, but longer-term studies had not yet been published. This multicenter randomized clinical trial (IXORA-PEDS) was conducted from May to October 2021 and evaluated the response and safety of the drug for 108 weeks. The patients had a mean (SD) age of 13.5 (3.04) years. 139 (83.7%) patients completed week 108. Primary and gated secondary end points that were achieved by week 12 were sustained through week 108, with patients achieving or maintaining PASI (Psoriasis Area and Severity Index) of 75 (91.7% [n = 86]) and sPGA (static Physician’s Global Assessment) 0 or 1 (78.3% [n = 74]). Clearance of nail psoriasis increased from 22.8% (n = 28) at week 12 to 68.1% (n = 28) at week 108. Similarly, clearance of palmoplantar psoriasis increased from 46.2% (n = 13) at week 12 to 90.0% (n = 10) at week 108, and clearance of scalp psoriasis increased from 70.7% (n = 83) at week 12 to 76.2% (n = 83) at week 108. A total of 90.9% of patients (n = 30) who received placebo relapsed, compared with 17.6% of patients (n = 6) who were treated with ixekizumab. No new Candida infections or anaphylaxis episodes were reported from weeks 48 to 108. Treatment with ixekizumab continued to be effective for long-term management of psoriasis in children with no apparent increased safety risks.
How well can you monitor response to imiquimod with in vivo reflectance confocal microscopy?
Journal of the American Academy of Dermatology
Lentigo maligna (LM), an ‘in situ’ form of melanoma, can pose a treatment challenge when Mohs surgery is unavailable and 5 mm margins would cause significant cosmetic disfigurement. In this case, imiquimod, a topical immunomodulator, is a reasonable alternative. For margin assessment, in vivo reflectance confocal microscopy (RCM), a noninvasive technique that images the skin, can be used by assigning a lentigo maligna score (LMS). In this RCT of 40 patients, the authors sought to determine the accuracy of LMS score 1 month after imiquimod treatment. The results showed that the lower LMS score at 1 month was statistically significant (P < 0.001), and the 4 criteria that were significantly decreased included 1) non edged papillae (68% of LM; OR 10.5), 2) large rounded pagetoid cells >20um (37%; OR, 10.3) , 3) 3+ atypical cells at the DEJ in 5 images (86%, OR 13.8), and a follicular spread of pagetoid cells (59%; OR, 7.8). Histologic clearance of the tumor was observed in 52% of patients and the RCM examination showed an LMS of <2 in 48% of patients. No false-negative results were obtained by RCM regarding LM diagnosis and margin analysis. Limitations include small sample size; Future studies should increase frequency and duration of imiquimod application. This study shows that RCM can be used as an adjunctive tool for assessing LM response to various treatments, including presurgical evaluation and treatment follow-up.
Using the microbiome to detect skin cancer
Journal of Investigative Dermatology
We’re headed back to exploring the skins’ microbiome this week, but this time we are investigating how it changes in cancerous states. In particular, researchers were curious if there was a difference in the microbiota for those with actinic keratosis (AK) or squamous cell carcinoma (SCC) compared to healthy skin. 81 patients with AK and/or SCC, and 25 controls were recruited for this study; a total of 336 samples were analyzed. Samples collected from cancerous sites were control matched based on age, gender, and sample site. Results showed a significant decrease in the ratio of Cutibacterium acnes:Staphylococcus aureus in SCC samples, and a downward trend in AK samples. These findings are particularly interesting because previous studies showed that C. acnes is antitumorigenic, while S. aureus promotes tumor cell growth. The authors postulate that the shift in species ratio might play a role in cancer progression. One limitation is that the findings are correlational, and do not determine if the change in microbiome promotes cancerous states, or if cancer cells play a role in shifting the microbiota. Nonetheless, these findings are exciting because they suggest the microbiome may be a useful biomarker for detecting skin cancer in the future.
JAMA Dermatology
Don’t forget about the kiddos! Psoriasis affects about 1% of children and can have significant effects on their quality of life, as well as multiple comorbidities. Ixekizumab is approved as a first-line option for treatment of moderate to severe psoriasis in children ages 6-18 years old. Prior studies had shown this to be superior to placebo, but longer-term studies had not yet been published. This multicenter randomized clinical trial (IXORA-PEDS) was conducted from May to October 2021 and evaluated the response and safety of the drug for 108 weeks. The patients had a mean (SD) age of 13.5 (3.04) years. 139 (83.7%) patients completed week 108. Primary and gated secondary end points that were achieved by week 12 were sustained through week 108, with patients achieving or maintaining PASI (Psoriasis Area and Severity Index) of 75 (91.7% [n = 86]) and sPGA (static Physician’s Global Assessment) 0 or 1 (78.3% [n = 74]). Clearance of nail psoriasis increased from 22.8% (n = 28) at week 12 to 68.1% (n = 28) at week 108. Similarly, clearance of palmoplantar psoriasis increased from 46.2% (n = 13) at week 12 to 90.0% (n = 10) at week 108, and clearance of scalp psoriasis increased from 70.7% (n = 83) at week 12 to 76.2% (n = 83) at week 108. A total of 90.9% of patients (n = 30) who received placebo relapsed, compared with 17.6% of patients (n = 6) who were treated with ixekizumab. No new Candida infections or anaphylaxis episodes were reported from weeks 48 to 108. Treatment with ixekizumab continued to be effective for long-term management of psoriasis in children with no apparent increased safety risks.
How well can you monitor response to imiquimod with in vivo reflectance confocal microscopy?
Journal of the American Academy of Dermatology
Lentigo maligna (LM), an ‘in situ’ form of melanoma, can pose a treatment challenge when Mohs surgery is unavailable and 5 mm margins would cause significant cosmetic disfigurement. In this case, imiquimod, a topical immunomodulator, is a reasonable alternative. For margin assessment, in vivo reflectance confocal microscopy (RCM), a noninvasive technique that images the skin, can be used by assigning a lentigo maligna score (LMS). In this RCT of 40 patients, the authors sought to determine the accuracy of LMS score 1 month after imiquimod treatment. The results showed that the lower LMS score at 1 month was statistically significant (P < 0.001), and the 4 criteria that were significantly decreased included 1) non edged papillae (68% of LM; OR 10.5), 2) large rounded pagetoid cells >20um (37%; OR, 10.3) , 3) 3+ atypical cells at the DEJ in 5 images (86%, OR 13.8), and a follicular spread of pagetoid cells (59%; OR, 7.8). Histologic clearance of the tumor was observed in 52% of patients and the RCM examination showed an LMS of <2 in 48% of patients. No false-negative results were obtained by RCM regarding LM diagnosis and margin analysis. Limitations include small sample size; Future studies should increase frequency and duration of imiquimod application. This study shows that RCM can be used as an adjunctive tool for assessing LM response to various treatments, including presurgical evaluation and treatment follow-up.
Using the microbiome to detect skin cancer
Journal of Investigative Dermatology
We’re headed back to exploring the skins’ microbiome this week, but this time we are investigating how it changes in cancerous states. In particular, researchers were curious if there was a difference in the microbiota for those with actinic keratosis (AK) or squamous cell carcinoma (SCC) compared to healthy skin. 81 patients with AK and/or SCC, and 25 controls were recruited for this study; a total of 336 samples were analyzed. Samples collected from cancerous sites were control matched based on age, gender, and sample site. Results showed a significant decrease in the ratio of Cutibacterium acnes:Staphylococcus aureus in SCC samples, and a downward trend in AK samples. These findings are particularly interesting because previous studies showed that C. acnes is antitumorigenic, while S. aureus promotes tumor cell growth. The authors postulate that the shift in species ratio might play a role in cancer progression. One limitation is that the findings are correlational, and do not determine if the change in microbiome promotes cancerous states, or if cancer cells play a role in shifting the microbiota. Nonetheless, these findings are exciting because they suggest the microbiome may be a useful biomarker for detecting skin cancer in the future.
QUESTION OF THE WEEK
NEJM CHALLENGE QUESTION
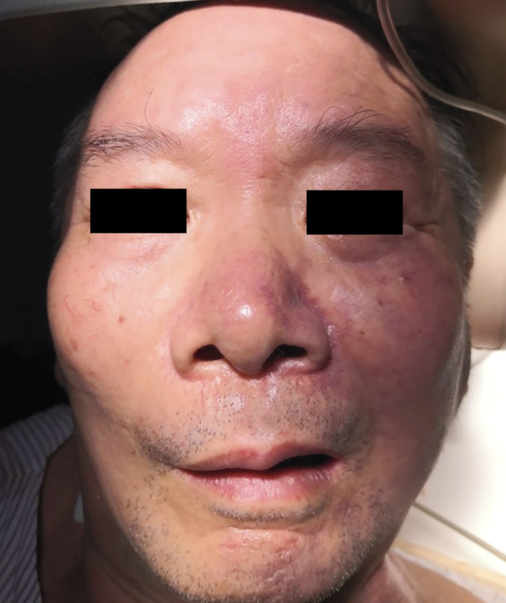
A 63-year-old man developed purplish discoloration of his face after he underwent stenting and balloon dilation of the left common carotid artery. Cholesterol embolization syndrome was diagnosed. What is the name of this physical exam finding?
1. Cutis marmorata
2. Harlequin syndrome
3. Livedo racemosa
4. Livedo reticularis
5. Telangiectasia
Answer: Livedo reticularis
He developed purplish discoloration on face after stenting and balloon dilation of left common carotid artery. He subsequently had shivering, sweating and confusion and developed a left gaze preference, dysarthria and hemiparesis on the right side of body. Over next 20 minutes, livedo reticularis developed on the left side of his face. This finding was due to his diagnosis of acute embolic stroke and cholesterol embolization syndrome. In cholesterol embolization syndrome, atherosclerotic plaques from large arteries embolize to smaller arteries, which leads to vascular occlusion, inflammation, and end-organ damage. Livedo reticularis (which is shown in this picture) is one of the most common cutaneous manifestation.
Other answers:
1. Cutis marmorata - condition where the skin has a pinkish blue mottled or marbled appearance when subjected to cold temperatures; cutis marmorata telangiectatica congenita is an entity that is present at birth as reticulated erythematous-violaceous vascular network that is usually unilateral on lower extremities. It typically fades over 2-3 years, however before then it can ulcerate/atrophy and scar.
2. Harlequin syndrome - condition characterized by asymmetric sweating and flushing on the upper thoracic region of the chest, neck and face. Harlequin syndrome is considered an injury to the autonomic nervous system (ANS).
3. Livedo racemosa - physical exam finding that consists of erythematous/violaceous discoloration of skin that consists of larger branching network and incomplete rings (vs smaller complete rings of LR)
5. Telangiectasia - dilated or broken blood vessels located near the surface of the skin or mucous membranes.
He developed purplish discoloration on face after stenting and balloon dilation of left common carotid artery. He subsequently had shivering, sweating and confusion and developed a left gaze preference, dysarthria and hemiparesis on the right side of body. Over next 20 minutes, livedo reticularis developed on the left side of his face. This finding was due to his diagnosis of acute embolic stroke and cholesterol embolization syndrome. In cholesterol embolization syndrome, atherosclerotic plaques from large arteries embolize to smaller arteries, which leads to vascular occlusion, inflammation, and end-organ damage. Livedo reticularis (which is shown in this picture) is one of the most common cutaneous manifestation.
Other answers:
1. Cutis marmorata - condition where the skin has a pinkish blue mottled or marbled appearance when subjected to cold temperatures; cutis marmorata telangiectatica congenita is an entity that is present at birth as reticulated erythematous-violaceous vascular network that is usually unilateral on lower extremities. It typically fades over 2-3 years, however before then it can ulcerate/atrophy and scar.
2. Harlequin syndrome - condition characterized by asymmetric sweating and flushing on the upper thoracic region of the chest, neck and face. Harlequin syndrome is considered an injury to the autonomic nervous system (ANS).
3. Livedo racemosa - physical exam finding that consists of erythematous/violaceous discoloration of skin that consists of larger branching network and incomplete rings (vs smaller complete rings of LR)
5. Telangiectasia - dilated or broken blood vessels located near the surface of the skin or mucous membranes.