TWENTY-THIRD ISSUE
december 7, 2022
Needle little more information on dupilumab?
We all know dupilumab, the wonder drug for atopic dermatitis, but little is known regarding the associations between its serum levels with efficacy or adverse effects. Typically, adults with atopic dermatitis who are prescribed dupilumab receive a standard dose of 300 mg biweekly.
This prospective cohort study measured serum dupilumab levels and Eczema Area and Severity Index (EASI) scores at week 16 of treatment with 600 mg loading dose of dupilumab, followed by 300 mg injections every two weeks. At week 52, EASI score was calculated for comparison to baseline scores. Dupilumab-associated adverse effects were documented throughout the treatment course. Multivariate logistic regression was used to evaluate correlation between serum dupilumab levels and treatment response, as well as adverse effects.
Of 295 patients, the median serum dupilumab level was 86.6 μg/mL (range: 10.1-382.0 μg/mL). When stratified by week 16 EASI status, no significant differences in serum dupilumab levels were detected. Odds ratios (ORs) for prediction of response at 52 weeks based on week 16 serum dupilumab levels were insignificant (EASI 90: OR, 0.96 [95% CI, 0.90-1.04; P = .34] and EASI 75: OR, 1.03 [95% CI, 0.93-1.14; P = .55]). Correlation between week 16 levels and adverse effects was also insignificant (OR, 1.01 [95% CI, 0.95-1.07; P = .83]).
Limitations: Measurements of serum dupilumab were performed independent of dupilumab administration.
Main Takeaways: Despite a wide range of serum dupilumab levels at week 16, there was no association with treatment response or adverse effects within the first year of treatment.
We all know dupilumab, the wonder drug for atopic dermatitis, but little is known regarding the associations between its serum levels with efficacy or adverse effects. Typically, adults with atopic dermatitis who are prescribed dupilumab receive a standard dose of 300 mg biweekly.
This prospective cohort study measured serum dupilumab levels and Eczema Area and Severity Index (EASI) scores at week 16 of treatment with 600 mg loading dose of dupilumab, followed by 300 mg injections every two weeks. At week 52, EASI score was calculated for comparison to baseline scores. Dupilumab-associated adverse effects were documented throughout the treatment course. Multivariate logistic regression was used to evaluate correlation between serum dupilumab levels and treatment response, as well as adverse effects.
Of 295 patients, the median serum dupilumab level was 86.6 μg/mL (range: 10.1-382.0 μg/mL). When stratified by week 16 EASI status, no significant differences in serum dupilumab levels were detected. Odds ratios (ORs) for prediction of response at 52 weeks based on week 16 serum dupilumab levels were insignificant (EASI 90: OR, 0.96 [95% CI, 0.90-1.04; P = .34] and EASI 75: OR, 1.03 [95% CI, 0.93-1.14; P = .55]). Correlation between week 16 levels and adverse effects was also insignificant (OR, 1.01 [95% CI, 0.95-1.07; P = .83]).
Limitations: Measurements of serum dupilumab were performed independent of dupilumab administration.
Main Takeaways: Despite a wide range of serum dupilumab levels at week 16, there was no association with treatment response or adverse effects within the first year of treatment.
Increased incidence of atopic dermatitis is associated with increased long-term exposure to air particulate matter
Journal of The American Academy of Dermatology
When fresh air might not be so good for you…
Atopic dermatitis (AD), also known as eczema, is the most common inflammatory skin condition worldwide with a lifetime prevalence of >15%. Exposure to air pollutants, including ambient particulate matter (PM), a combination of microscopic solid and liquid particles that can penetrate the skin, have been thought to exacerbate AD, but researchers sought to evaluate more specifically how PM may affect the risk of developing AD over time.
In this retrospective cohort study, researchers analyzed 209,168 subjects from the Korean National Health Insurance Service-National Sample Cohort (NHIS-NSC) who were assigned the ICD-10 code for AD. Patients who were treated for AD or its related comorbidities prior to the study period were excluded. At 313 meteorological sites, ambient particulate matter and gaseous air pollution were measured hourly. The site closest to the residence of each subject was used to measure average pollutant concentrations, and long-term average concentration of air pollutants per subject was calculated.
Results showed that 1,030,324 person-years of air pollutant risk yielded 3203 new cases of AD (310.9/100,000 person-year). The age group with the highest incidence of AD was 0 years (42.59%), followed by 5-9 years (6.99%), and 1-4 years (5.87%). Analysis also showed significant positive association between long-term average concentration of PM2.5 (hazard ratio [HR], 1.420; 95% CI, 1.392-1.448; for 1 µg/m3), PM10 (HR, 1.333; 95% CI, 1.325-1.341; for 1 µg/m3), SO2 (HR, 1.626; 95% CI, 1.559-1.695; for 1 part per billion [ppb]), NO2 (HR, 1.200; 95% CI, 1.187-1.212; for 1 ppb), and CO (HR, 1.005; 95% CI, 1.004-1.005; for 1 ppb) and incidence of AD.
Limitations: Lack of detailed patient information in NHIS-NSC, an anonymized database.
Main Takeaways: Long-term increased exposure to ambient air particulates was significantly associated with increased risk of AD development.
Atopic dermatitis (AD), also known as eczema, is the most common inflammatory skin condition worldwide with a lifetime prevalence of >15%. Exposure to air pollutants, including ambient particulate matter (PM), a combination of microscopic solid and liquid particles that can penetrate the skin, have been thought to exacerbate AD, but researchers sought to evaluate more specifically how PM may affect the risk of developing AD over time.
In this retrospective cohort study, researchers analyzed 209,168 subjects from the Korean National Health Insurance Service-National Sample Cohort (NHIS-NSC) who were assigned the ICD-10 code for AD. Patients who were treated for AD or its related comorbidities prior to the study period were excluded. At 313 meteorological sites, ambient particulate matter and gaseous air pollution were measured hourly. The site closest to the residence of each subject was used to measure average pollutant concentrations, and long-term average concentration of air pollutants per subject was calculated.
Results showed that 1,030,324 person-years of air pollutant risk yielded 3203 new cases of AD (310.9/100,000 person-year). The age group with the highest incidence of AD was 0 years (42.59%), followed by 5-9 years (6.99%), and 1-4 years (5.87%). Analysis also showed significant positive association between long-term average concentration of PM2.5 (hazard ratio [HR], 1.420; 95% CI, 1.392-1.448; for 1 µg/m3), PM10 (HR, 1.333; 95% CI, 1.325-1.341; for 1 µg/m3), SO2 (HR, 1.626; 95% CI, 1.559-1.695; for 1 part per billion [ppb]), NO2 (HR, 1.200; 95% CI, 1.187-1.212; for 1 ppb), and CO (HR, 1.005; 95% CI, 1.004-1.005; for 1 ppb) and incidence of AD.
Limitations: Lack of detailed patient information in NHIS-NSC, an anonymized database.
Main Takeaways: Long-term increased exposure to ambient air particulates was significantly associated with increased risk of AD development.
Timely Wound Healing Is Dependent on Endothelial but Not on Hair Follicle Stem Cell Toll-Like Receptor 2 Signaling
Journal of Investigative Dermatology
TLR stem cells: Time’s not the only thing that heals all wounds!
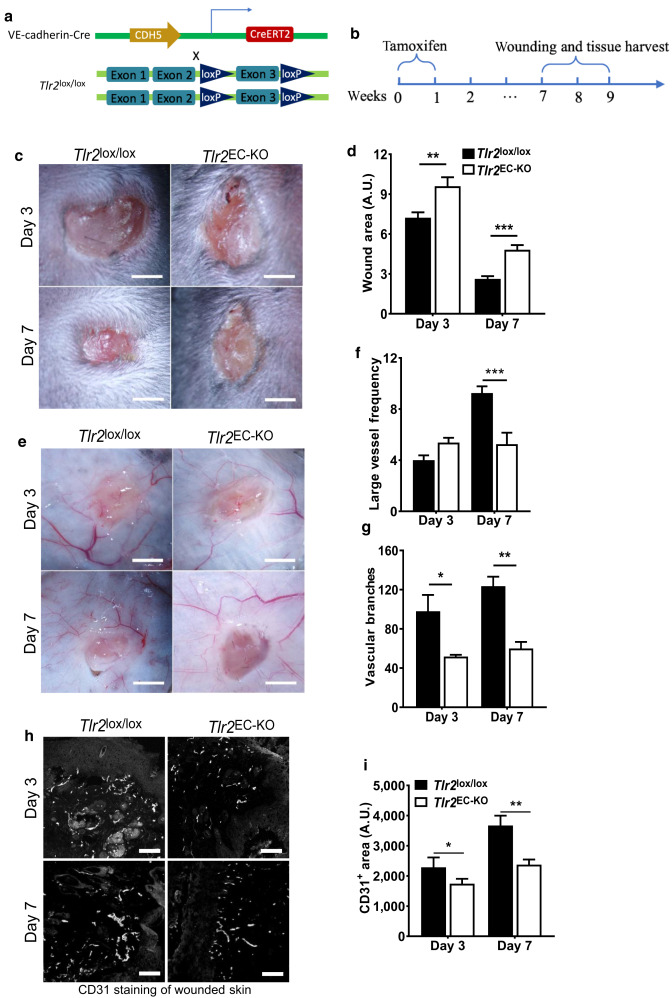
Toll-like receptors (TLR), members of the innate immune system, play a prominent role in wound healing and subsequently stimulate stem cells. The major source of stem cells is from the basal layer of the epidermis and the bulge region of the hair follicles (HFSC). In this study, they used Cre-loxP inducible recombination technology to create Tlr2-knockout mouse lines to distinguish the roles of endothelial TLR2 and HFSC TLR2 in wound healing. Endothelial tlr2-knockout (Tlr2EC-KO) mice were induced using tamoxifen, which targets this process. The HFSC tlr-2 knockout (Tlr2HFSC-KO) mice were induced by Ker15 promoter‒driven Cre recombinase, with the deltion confirmed by western blot. Dorsal skin of mice was shaved and sterilized. A 6-mm biopsy punch was used to create the wounds.
Three days and 7 days after injury, Tlr2EC-KO mice showed a significantly larger wound area than their control Tlr2lox/lox littermates, with the wound area being approximately two times larger on day 7. In those stimulated with endothelial-tlr2, there was an increased proliferation and sprouting of vessels in the thoracic aorta of the mice, as well as an increased number of proangiogenic factors, responsible for this increased angiogenesis seen with endothelial stimulation. There were no significant differences in wound closure on day 4 or day 7 between Tlr2HFSC-KO and the control. TLR2 deletion in keratinocytes had no effect on keratinocyte proliferation.
Main Takeaways: Endothelial TLR stem cells play a significantly more important role in the pathogenesis of healing than TLR stem cells from hair follicles.
Postoperative wound healing after fractionated ablative resurfacing improves with macrophage-acting gels
Dermatologic Surgery
Dermatologic Surgery
Who do you call if you want to get rid of your wrinkles? Iron man!
Fractionated ablative resurfacing can be used to improve the appearance of UV-induced photodamage, rhytids, dyspigmentation, and suboptimal skin texture. Post-operative skin care is important in promoting optimal wound healing and cosmetic outcomes after laser therapy. Numerous topical medications have been used post-operatively, but there is currently no gold standard agent. A novel macrophage-activating (TR-987 0.1%) gel is a topical drug candidate that activates pattern recognition receptors on immune cells to stimulate tissue repair and regeneration, leading to enhanced wound healing.
Researchers conducted a prospective, Phase 2B double-blind, placebo-controlled, randomized clinical trial of 42 patients between ages 45 and 65 with baseline chest wrinkling class of II or greater and elastosis score of 6 or greater. All subjects underwent a standardized fractionated CO2 laser resurfacing treatment to the chest. After ablative laser resurfacing of the chest, patients were randomly divided to receive either the TR-987 0.1% active gel or a placebo gel. The full tube of gel was applied daily for a total of 5 applications, after which all subjects were transitioned to routine standard of care (daily cleansing and 1% dimethicone ointment). Blind evaluators assessed skin quality across wrinkling and elastosis using the Fitzpatrick-Goldman Wrinkle Scale (FGWS). At day 28, 85% of subjects in the TR-987 0.1% gel group achieved an improvement of at least 33% in skin quality, compared to 50% in the placebo group. Additionally, 75% of subjects in the TR-987 0.1% gel group achieved an improvement of at least 33% in elastosis at day 28, compared to 33% in the placebo group.
Limitations: Further studies are needed to investigate the long-term results on wrinkling from use of the TR-987 gel.
Main Takeaway: This study confirms the effects of novel macrophage-activating gel for acceleration and optimization of skin healing after laser resurfacing of the chest.
innovations in dermatology
I’m not blushing, it's just Rosacea!
Rosacea is a multifactorial skin disease that presents as inflammation, flushing, and telangiectasias of the face. Treatments are often unsatisfactory given the lack of significant resolution of symptoms. Erythematotelangiectatic rosacea (ETR) is the most common subtype of rosacea, yet it is the most difficult to treat. Current ETR treatments utilize intense pulsed light (IPL) to condense capillaries and enhance remodeling of dermal collagen to then reduce inflammation, but there is increased risk for skin burns. Safer treatments stem from the use of Photoelectric Therapy (OPT) which has shown to be effective in promoting epidermal repair/regeneration via the proliferation of fibroblasts as well as inhibiting expression of inflammatory mediators.
A novel treatment for ETR was proposed utilizing optimal pulse technology (OPT) with low energy, three pulses, and a long pulse width, known as advanced OPT (AOPT-LTL) to more adequately relieve erythema and inflammation. Both a mouse model and small clinical study were utilized to evaluate the efficacy and safety of AOPT-LTL.
The erythema and capillary density in dermoscopic images were scored before and after treatment and showed a significant improvement (p<0.05 and p<0.01 respectively). ADOPT-LTL treatment also showed a significant (p<0.01) decrease in the total number of inflammatory cells per high powered field (HPF). The expression of camp, kallikrein 5 and toll-like receptor 2 which was used to simulate the molecular mechanism of rosacea were significantly (p<0.01) downregulated following treatment. AOPT-LTL was also found to have a regulatory effect on vascular and neurological dysfunction in rosacea. All patients who completed the treatment and follow up showed improvement in their condition based on photo representation. During the three month follow up period, some patients showed slight recurrence but there was still significant improvement from baseline. Consequently, AOPT-LTL can improve the symptoms of ETR and is a safe and effective treatment to continue to explore in future clinical trial studies.
Limitations: Small sample size of patients and short time frame of study do not show the widespread or long term effects of the treatment.
Main Takeaway: AOPT-LTL can improve the symptoms of ETR and is a safe and effective treatment to continue to explore in future clinical trial studies
Rosacea is a multifactorial skin disease that presents as inflammation, flushing, and telangiectasias of the face. Treatments are often unsatisfactory given the lack of significant resolution of symptoms. Erythematotelangiectatic rosacea (ETR) is the most common subtype of rosacea, yet it is the most difficult to treat. Current ETR treatments utilize intense pulsed light (IPL) to condense capillaries and enhance remodeling of dermal collagen to then reduce inflammation, but there is increased risk for skin burns. Safer treatments stem from the use of Photoelectric Therapy (OPT) which has shown to be effective in promoting epidermal repair/regeneration via the proliferation of fibroblasts as well as inhibiting expression of inflammatory mediators.
A novel treatment for ETR was proposed utilizing optimal pulse technology (OPT) with low energy, three pulses, and a long pulse width, known as advanced OPT (AOPT-LTL) to more adequately relieve erythema and inflammation. Both a mouse model and small clinical study were utilized to evaluate the efficacy and safety of AOPT-LTL.
The erythema and capillary density in dermoscopic images were scored before and after treatment and showed a significant improvement (p<0.05 and p<0.01 respectively). ADOPT-LTL treatment also showed a significant (p<0.01) decrease in the total number of inflammatory cells per high powered field (HPF). The expression of camp, kallikrein 5 and toll-like receptor 2 which was used to simulate the molecular mechanism of rosacea were significantly (p<0.01) downregulated following treatment. AOPT-LTL was also found to have a regulatory effect on vascular and neurological dysfunction in rosacea. All patients who completed the treatment and follow up showed improvement in their condition based on photo representation. During the three month follow up period, some patients showed slight recurrence but there was still significant improvement from baseline. Consequently, AOPT-LTL can improve the symptoms of ETR and is a safe and effective treatment to continue to explore in future clinical trial studies.
Limitations: Small sample size of patients and short time frame of study do not show the widespread or long term effects of the treatment.
Main Takeaway: AOPT-LTL can improve the symptoms of ETR and is a safe and effective treatment to continue to explore in future clinical trial studies