Tenth Issue
May 18th, 2022
A new evaluation tool for ichthyosis vulgaris shows strong accuracy and potential for success
JAMA Dermatology
JAMA Dermatology
Ichthyosis vulgaris is a group of skin disorders classified by persistently dry, thickened, 'fish scale' skin.
- A group of investigators created a new evaluation tool, the Ichthyosis Scoring System (ISS), which was validated by several dermatologists
- The study found strong interrater and intrarater reliability, confirming the accuracy of the tool
- The success of this new evaluation tool can help aid in the management of patients with ichthyosis vulgaris, which often does not receive proper evaluation and treatment given its rarity
Some people have said that dermatologists actually practice itchcraft. Ichthyosis vulgaris is a group of skin disorders classified by persistently dry, thickened, 'fish scale' skin. A group of investigators created the Ichthyosis Scoring System (ISS), which contains more extensive descriptors and additional information on the impact of quality of life compared to prior evaluation tools. A thorough review of professional photographs from reputable sources was reviewed by experts who selected 56 images and written definitions to serve as standards for raters. The ISS also included more skin images from individuals of other ethnicities and races, including Asian, Black, and Hispanic populations compared with prior severity scoring systems. It was subsequently validated by several dermatologists via interrater and intrarater reliability. In the first cohort, ICC agreement for the total score was 0.903 (95% CI, 0.770-0.974) and interrater reliabilities for erythema were moderate to excellent regardless of site. There were similar results for intrarater reliability. In the first cohort, soles exhibited the highest ICCs for scale during both rounds of testing while elbows and lower extremities were among the most challenging sites to assess in both cohorts. The success of this new evaluation tool can help aid in the management of patients with ichthyosis vulgaris, which often does not receive proper evaluation and treatment given its rarity.
How do TNF alpha inhibitors in combination with systemic steroids improve outcomes for SJS/TEN management?
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Steven Johnson Syndrome (SJS) and Toxic Epidermal necrolysis (TEN) refer to a life threatening dermatologic condition which presents with erythema and blistering, resulting in widespread epidermal detachment (think skin “sloughing”). Unfortunately, treatment is controversial and no standardized treatment protocol exists.
It’s a dermatologic emergency…for real! While they may take the brunt of many “dermatology emergency” jokes, Steven Johnson Syndrome (SJS) and Toxic Epidermal necrolysis (TEN) are no joke!
SJS/TEN refer to a life threatening dermatologic condition which presents with erythema and blistering, resulting in widespread epidermal detachment (think skin “sloughing”). SJS/TEN occur on a spectrum depending on how much denuded skin is involved (SJS <10%, overlap of SJS/TEN 10-30%, TEN >30%). For a condition that has such a high mortality rate, the best treatment regimen is controversial and no standard treatment guidelines exist. Traditional treatments have included steroids, IVIG and cyclosporine, and more recently TNF alpha inhibitors. This prospective study explores the role of TNF alpha inhibitors combined with systemic steroids in the management of SJS/TEN by comparing 10 patients who received methylprednisolone only versus 15 patients who received methylprednisolone (equiv to 1- 1.5 mg/kg/day prednisolone) and TNF alpha inhibitors (etanercept, 25 mg twice a week until steroid tapering).
What did they find?
Limitations of this study include the small sample size. While treatment with SJS/TEN still lacks standard guidelines, this study suggests that TNF alpha inhibitors in combination with systemic steroids could shorten clinical duration of disease by acute duration and skin healing time.
High yield fact: there are three main types of TNF alpha inhibitors:
- Prospective study comparing healing time and cytokine levels in patients with SJS/TENS receiving systemic steroids only (methylprednisolone) (n=10) versus steroids + TNF alpha inhibitor (Etanercept ) (n=15)
- Patients receiving steroids + etanercept had significantly shorter courses of initial steroid use, acute stage of disease, skin healing time and hospitalization time. No shorter time in mucosal healing was found between two groups
- Patients treated steroids + etanercept had significantly lower levels of IL-6, IL-18, MIP-1𝛂 in addition to IL-15 found in the steroid only group
- IL-6 is likely a biomarker that predicts clinical course for patients treated with steroids + TNF alpha inhibitors
It’s a dermatologic emergency…for real! While they may take the brunt of many “dermatology emergency” jokes, Steven Johnson Syndrome (SJS) and Toxic Epidermal necrolysis (TEN) are no joke!
SJS/TEN refer to a life threatening dermatologic condition which presents with erythema and blistering, resulting in widespread epidermal detachment (think skin “sloughing”). SJS/TEN occur on a spectrum depending on how much denuded skin is involved (SJS <10%, overlap of SJS/TEN 10-30%, TEN >30%). For a condition that has such a high mortality rate, the best treatment regimen is controversial and no standard treatment guidelines exist. Traditional treatments have included steroids, IVIG and cyclosporine, and more recently TNF alpha inhibitors. This prospective study explores the role of TNF alpha inhibitors combined with systemic steroids in the management of SJS/TEN by comparing 10 patients who received methylprednisolone only versus 15 patients who received methylprednisolone (equiv to 1- 1.5 mg/kg/day prednisolone) and TNF alpha inhibitors (etanercept, 25 mg twice a week until steroid tapering).
What did they find?
- Patients receiving steroids + etanercept had significantly shorter courses of initial steroid use, acute stage of disease, skin healing time and hospitalization. No shorter time in mucosal healing was found between two groups
- Patients treated with steroids + etanercept had significantly lower levels of more cytokines than the steroid only group (which only showed decreased levels of IL-15), including IL-6, IL-18, MIP-1𝛂.
- IL-6 is likely a biomarker that predicts clinical course for patients treated wtih steroids + TNF alpha inhibitors
Limitations of this study include the small sample size. While treatment with SJS/TEN still lacks standard guidelines, this study suggests that TNF alpha inhibitors in combination with systemic steroids could shorten clinical duration of disease by acute duration and skin healing time.
High yield fact: there are three main types of TNF alpha inhibitors:
- Adalimumab (brand name=Humira)- subcutaneous injection of fully human monoclonal IgG antibody against transmembrane TNF-receptor
- Infliximab (brand name= Remicade/Inflectra)- intravenous injection of chimeric monoclonal IgG antibody binding TNF-α only (targets soluble and transmembrane TNF-receptor)
- Etanercept (brand name= Enbrel)- subcutaneous injection of fully human dimeric fusion protein (TNF-receptor linked to Fc portion of IgG) that binds both TNF-α (soluble and membrane-bound) and TNF-β
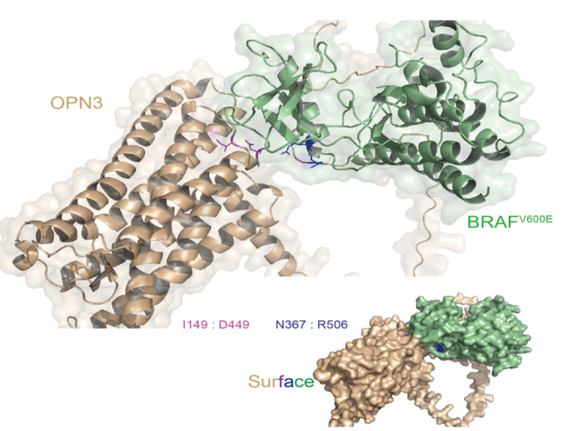
Opsin 3 (OPN3) is a negative regulator of melanogenesis in BRAFV600E mutated congenital melanocytic nevi, helping us understand the mechanism of action of melanogenesis in such lesions.
Maybe she’s born with it, maybe it’s…. a congenital melanocytic nevus? Congenital melanocytic nevus (CMN) is a common type of nevus that is present at birth. Caused by somatic mutations in utero, it has been established that BRAFV600E is the dominant mutation for small CMN. The aim of this study is to explore the role that opsin 3 (OPN3), a g-protein-coupled receptor, plays in the regulation of melanogenesis for CMN. 53 CMN tissue samples were collected, 27 from non-BRAFV600E and 26 from BRAFV600E samples. Researchers found a negative correlation between OPN3 expression and melanin density in BRAFV600E nevi, meaning that OPN3 expression reduced melanin production. Further, using siRNA scientists knocked out OPN3 in BRAFV600E cells and found a significant increase in melanin production, again showing its role as a negative regulator. They additionally found that OPN3 works to mediate melanogenesis through the BRAFV600E/extracellular regulated protein kinase signaling pathway. These findings are significant because they help to elucidate the mechanism of melanogenesis in BRAFV600E CMNs and may aid in future development of treatment options.
- 53 CMN tissue samples were collected, 27 from non-BRAFV600E and 26 from BRAFV600E samples
- A negative correlation between OPN3 expression and melanin density in BRAFV600E nevi was found, meaning that OPN3 expression reduced melanin production
- Knocking out OPN3 in BRAFV600E cells and found a significant increase in melanin production
- Findings elucidate mechanism of melanogenesis in BRAFV600E CMNs and may aid in future development of treatment options
Maybe she’s born with it, maybe it’s…. a congenital melanocytic nevus? Congenital melanocytic nevus (CMN) is a common type of nevus that is present at birth. Caused by somatic mutations in utero, it has been established that BRAFV600E is the dominant mutation for small CMN. The aim of this study is to explore the role that opsin 3 (OPN3), a g-protein-coupled receptor, plays in the regulation of melanogenesis for CMN. 53 CMN tissue samples were collected, 27 from non-BRAFV600E and 26 from BRAFV600E samples. Researchers found a negative correlation between OPN3 expression and melanin density in BRAFV600E nevi, meaning that OPN3 expression reduced melanin production. Further, using siRNA scientists knocked out OPN3 in BRAFV600E cells and found a significant increase in melanin production, again showing its role as a negative regulator. They additionally found that OPN3 works to mediate melanogenesis through the BRAFV600E/extracellular regulated protein kinase signaling pathway. These findings are significant because they help to elucidate the mechanism of melanogenesis in BRAFV600E CMNs and may aid in future development of treatment options.
QUESTION OF THE WEEK
NEJM CHALLENGE QUESTION
A 32-year-old man presented with itchy palmar lesions that appeared over the preceding 3 days. He had a similar episode 6 months earlier that resolved spontaneously. He has a history of recurrent oral herpes simplex infections. What is the diagnosis?
1. Herpes simplex virus infection
2. Mycoplasma pneumoniae infection
3. Chronic urticaria
4. Stevens–Johnson syndrome
5. Lupus erythematosus
1. Herpes simplex virus infection
2. Mycoplasma pneumoniae infection
3. Chronic urticaria
4. Stevens–Johnson syndrome
5. Lupus erythematosus
Answer: Herpes simplex virus infection
Physical examination shows targetoid lesions on the palmar surfaces. There was no mucosal involvement, however there were subtle erosions on vermillion border of lip consistent with resolving herpes infection. The lesions on the palms were consistent with erythema multiforme, a condition that may develop in response to certain infections (most commonly herpes simplex virus) but that may also be associated with certain medications or autoimmune conditions. At a follow-up visit 7 days after presentation, the lesions had resolved without specific treatment.
Erythema multiforme high yield facts*:
- 90% are caused by infection (HSV 1> HSV2, mycoplasma pneumonia >> histoplasma)
- Other causes include medications, radiation, idiopathic or chronic oral
- Clinical presentation typically presents with targetoid lesions with three zones
- Dusky, vascular, or necrotic center
- Elevated, edematous pale surrounding ring
- Outer rim of macular erythema
- EM minor= no systemic, minor mucosal involvement v EM major= systemic involvement and severe mucosal involvement
Other answers*:
2. Mycoplasma pneumoniae infection - presents with severe mucous membrane involvement (simulates SJS) and atypical papular target lesions; most common cause of EM major
3. Chronic urticaria - urticaria presents with wheals that come and go within 24 hours; chronic urticaria lasts >6 weeks (v acute urticaria <6 weeks)
4. Stevens–Johnson syndrome - presents with prodrome of systemic symptoms and clinically with atypical targetoid macules, erythema, and skin pain, which then results in dusky plaques with full-thickness sloughing; typically drug-induced (e.g. allopurinol, anticonvulsants etc)
5. Lupus erythematosus - there is an entity called Rowell’s syndrome which presents with targetoid lesions that resemble EM, however the patient also has lupus as well; typically Ro/SSA (+)
*Explanations developed with use of Alikhan, Ali, and Thomas LH Hocker. Review of Dermatology E-Book. Elsevier Health Sciences, 2017.
- 90% are caused by infection (HSV 1> HSV2, mycoplasma pneumonia >> histoplasma)
- Other causes include medications, radiation, idiopathic or chronic oral
- Clinical presentation typically presents with targetoid lesions with three zones
- Dusky, vascular, or necrotic center
- Elevated, edematous pale surrounding ring
- Outer rim of macular erythema
- EM minor= no systemic, minor mucosal involvement v EM major= systemic involvement and severe mucosal involvement
SK(IN DEPTH) RECAP
In Ahmady et al., which population of patients with actinic keratoses (AKs) had the highest risk of invasive cutaneous squamous cell carcinoma (cSCC)?
A. Grade 1
B. Grade 2
C. Grade 3
Which of the following AK treatments in Ahmady et al. was associated with the lowest 4-year risk of cSCC?
A. Florouracil
B. Imiquimod
C. Methylaminolevulinate PDT
D. Ingenol mebutate
In Winden et al, which was NOT found to be a predictive factor for basal cell carcinoma treatment burden?
A. Sex
B. Tumor size
C. Polypharmacy
D. Functionality (iADL dependency)
E. Age
In Werth et al., what was the effect of lenabasum on refractory cutaneous dermatomyositis?
A. Improvement in cutaneous dermatomyositis disease area and severity index (CDASI), significant side effects
B. Worsening of CDASI, significant side effects
C. Improvement in CDASI, well-tolerated
D. Worsening of CDASI, well-tolerated
A. Grade 1
B. Grade 2
C. Grade 3
Which of the following AK treatments in Ahmady et al. was associated with the lowest 4-year risk of cSCC?
A. Florouracil
B. Imiquimod
C. Methylaminolevulinate PDT
D. Ingenol mebutate
In Winden et al, which was NOT found to be a predictive factor for basal cell carcinoma treatment burden?
A. Sex
B. Tumor size
C. Polypharmacy
D. Functionality (iADL dependency)
E. Age
In Werth et al., what was the effect of lenabasum on refractory cutaneous dermatomyositis?
A. Improvement in cutaneous dermatomyositis disease area and severity index (CDASI), significant side effects
B. Worsening of CDASI, significant side effects
C. Improvement in CDASI, well-tolerated
D. Worsening of CDASI, well-tolerated
In Ahmady et al., which population of patients with actinic keratoses (AKs) had the highest risk of invasive cutaneous squamous cell carcinoma (cSCC)?
A. Grade 1
B. Grade 2
C. Grade 3
The authors examined the proportion of patients with invasive cSCC in prior areas of AKs. Olsen grade 1—slightly palpable AK, Olsen grade 2—moderately thick AK, and Olsen grade 3—very thick AK. They found the highest risk of invasive cSCC in patients with Olsen grade III AKs. Additionally, they found that the risk was even higher in patients who needed additional treatment.
Which of the following AK treatments in Ahmady et al. was associated with the lowest 4-year risk of cSCC?
A. Fluorouracil
B. Imiquimod
C. Methylaminolevulinate PDT
D. Ingenol mebutate
The 4-year risk of developing cSCC in a previously treated AK area was 3.7%. In patients treated with fluorouracil, the risk was 2.2%. Risk in patients treated with imiquimod, methylaminolevulinate PDT, and ingenol mebutate were 5.8%, 3.6%, and 3.0%, respectively.
In Winden et al, which was NOT found to be a predictive factor for basal cell carcinoma treatment burden?
A. Sex
B. Tumor size
C. Polypharmacy
D. Functionality (iADL dependency)
E. Age
The authors found that predictors of higher treatment burden included iADL dependency, female sex, larger tumor diameter, and polypharmacy. Interestingly, age was not significantly associated with outcomes.
In Werth et al., what was the effect of lenabasum on refractory cutaneous dermatomyositis?
A. Improvement in cutaneous dermatomyositis disease area and severity index (CDASI), significant side effects
B. Worsening of CDASI, significant side effects
C. Improvement in CDASI, well-tolerated
D. Worsening of CDASI, well-tolerated
Lenabasum targets CB2 receptors and is thought to reduce inflammatory responses. In this small cohort of patients randomized to lenabasum vs. placebo, they found that CDASI was improved in patients who received lenabasum. Additionally, they found that lenabasum was well-tolerated in this population.