TWELFTH ISSUE
June 15th, 2022
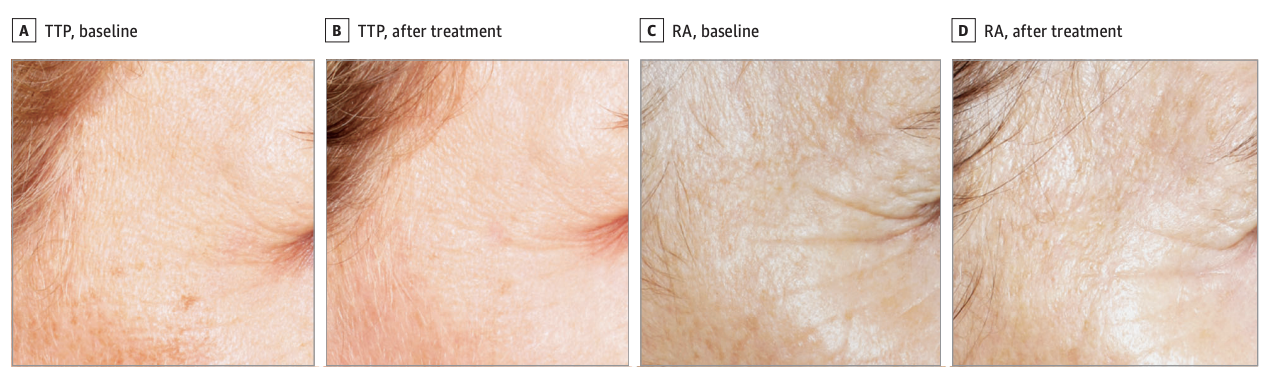
We all know tretinoin, famed for improving photodamaged skin by reducing wrinkles and treating dyspigmentation. While it is known that tretinoin can produce a more youthful appearance, it also causes many side effects such as erythema, pruritus, stinging, burning and scaling. It has long been theorized that the mechanism of action for retinoids induces procollagen I synthesis or suppresses expression of matrix metalloproteinases (most highly studied includes MMP1, MMP3, MMP9). Researchers set out to discover if tretinoin precursors had comparable anti-aging properties as tretinoin, and to explore the mechanism of action for retinoids. Twenty-four white participants (range 40-84 years, median 62 years; 22 females, 2 males) were randomized to use 0.02% tretinoin cream, or a 1.1% triple tretinoin precursor (TTP) that included retinol, retinyl acetate, and retinyl palmitate. Medication was applied to the entire face every other evening for the first 4 weeks, and every evening for the remaining 20 weeks. Biopsies were procured at baseline and at the end of the study, and clinical assessments were performed at 4, 12, 18 and 24 weeks. It was found that there was no clinically significant difference in improving the effects of photoaging between the two arms of the study (95% CI = -2 to 1; p= 0.27). Additionally, participants in the TTP group were blindly evaluated to have 6 times less erythema than the tretinoin treatment arm when evaluating side effects. Most surprisingly, there was not a significant induction procollagen I expression, or reduction in MMP1, MMP3, or MMP9 expression. Instead there was an observed suppression in MMP2, a less studied metalloproteinase, that degrades type IV collagen at the dermal-epidermal junction. Limitations of this study are small sample size, and almost entirely white, female patient population. Nonetheless, these findings are extremely significant because not only did they discover that TTPs are equally effective as tretinoin in reducing the effects of photo-aging, but likely discovered at least part of the mechanism of action of retinoids.
What are risk factors for poor outcomes in stage T2a squamous cell carcinomas?
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Never underestimate the little guy. In general, patients with cutaneous squamous cell carcinoma (CSCC), the second most common skin cancer, are cured with surgical excision alone. Although most complications with cutaneous squamous cell carcinoma occur with high-stage tumors (i.e. Brigham and Women’s Hospital (BWH) staging system T2b and T3- see table below), ~25% of low-stage tumors have poor outcomes (including nodal metastasis, distant metastasis and disease-specific deaths (DSD)). However, it is difficult to predict which ones will have a worse outcome. Since 30% of the negative sequelae in low-stage CSCC occur in BWH T2a tumors, the authors sought to investigate risk factors associated with poor outcomes in T2a tumors to better identify which ones to follow.
What did they find?
Limitations: potential for incomplete data (including histologic risk factors), has not been externally validated, low sensitivity of model (only 7.7%)
Main takeaway: BWH stage T2a-high CSCC tumors have an 8% chance of developing poor outcomes and should receive close clinical surveillance and may benefit from radiologic imaging
*cannot have overlapping category of risk factors in major and minor criteria (e.g. cannot have major criteria of poor differentiation and minor criteria of moderate differentiation)
What did they find?
- Multicenter retrospective chart review of 1342 stage T2a tumors over 17 years
- Very small proportion, 45 (3%), developed poor outcome
- BWH T2a-high tumors (the T2a tumors most at risk of developing poor outcomes) are defined by the presence of*:
- 1 major criterion (primary tumor diameter ≥40 cm, invasion depth beyond subcutaneous fat, poor differentiation, or large-caliber perineural invasion)
- ≥ 1 minor criterion (invasion depth in subcutaneous fat, moderate differentiation, small-caliber perineural invasion, or lymphovascular invasion)
- Based on this model, at 5 years, risk of a BWH T2a-high tumor developing a metastasis or causing a DSD is 8% v 2.8% in a T2a-low tumor (sensitivity of 7.7%, specificity of 97.4%)
Limitations: potential for incomplete data (including histologic risk factors), has not been externally validated, low sensitivity of model (only 7.7%)
Main takeaway: BWH stage T2a-high CSCC tumors have an 8% chance of developing poor outcomes and should receive close clinical surveillance and may benefit from radiologic imaging
*cannot have overlapping category of risk factors in major and minor criteria (e.g. cannot have major criteria of poor differentiation and minor criteria of moderate differentiation)
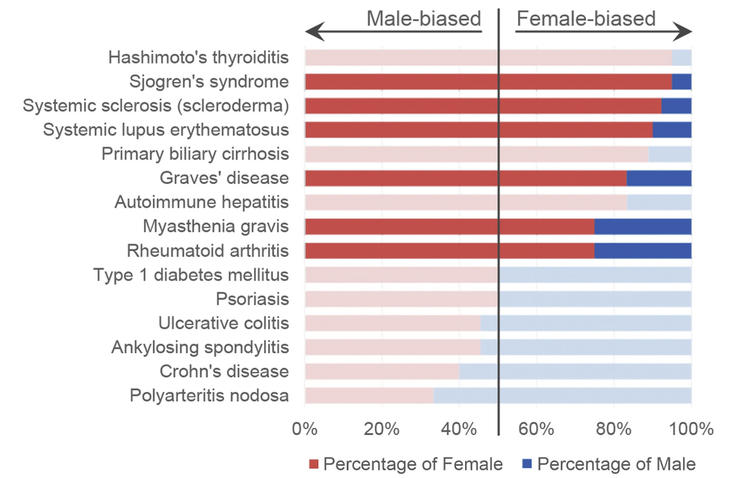
Why do we often associate autoimmune diseases with young women? Women are at increased risk for many autoimmune diseases, such as lupus, Sjogren’s, etc. There are likely several mechanisms at play in this female predisposition to autoimmunity. In this review by Xing et al., the authors examine the effects of hormones, X chromosome dosage and inactivation, and sex-biased genes on autoimmunity.
What did they find?
Limitations: Despite growth in our understanding of the female sex bias in autoimmunity, we still lack understanding on biologic male patients who develop female-predominant autoimmune disorders. Future studies are required to examine additional contributing factors to development of autoimmune disorders in general.
Main Take Away: There are biologic differences between males and females that contribute to the higher propensity of autoimmune diseases in biologic females. Better understanding of the molecular basis of autoimmune disease would aid in the development of more targeted therapies.
* Historically, a lot of animal research studies focused on male animals since they were thought to have less variability from reproductive cycles. However, recent insight into sex differences emphasize the importance of reporting and study.ing both sexes. The National Institutes of Health in 2016 said that sex as a biological variable should be included in both study design and analysis.
What did they find?
- Biologic women have stronger innate and adaptive immunity, which is good and bad because although it decreases susceptibility to infections, it likely plays a role in the increase in autoimmune disease incidence.
- Sex hormones affect the immune system, but it’s complicated. Progesterone and androgens tend to suppress the immune system while estrogen has a myriad of effects, which are ultimately thought to increase the immune response.
- To maintain equal amounts of genetic material, biologic females (XX) undergo X chromosome inactivation, but this does not affect all genes completely. The X chromosome harbors many immune genes, and the incompleteness of inactivation in women may play a role in amplifying immune responses.
- Certain genes (not regulated by hormones or found on X chromosomes) may be differentially expressed in biologic females. For example, VGLL3 was found to be upregulated in keratinocytes of women and serves as a transcription cofactor for many other genes involved in autoimmune diseases.
Limitations: Despite growth in our understanding of the female sex bias in autoimmunity, we still lack understanding on biologic male patients who develop female-predominant autoimmune disorders. Future studies are required to examine additional contributing factors to development of autoimmune disorders in general.
Main Take Away: There are biologic differences between males and females that contribute to the higher propensity of autoimmune diseases in biologic females. Better understanding of the molecular basis of autoimmune disease would aid in the development of more targeted therapies.
* Historically, a lot of animal research studies focused on male animals since they were thought to have less variability from reproductive cycles. However, recent insight into sex differences emphasize the importance of reporting and study.ing both sexes. The National Institutes of Health in 2016 said that sex as a biological variable should be included in both study design and analysis.
QUESTION OF THE WEEK
NEJM CHALLENGE QUESTION
A 40-year-old man presented with a 2-week history of scaly foot rash, joint swelling, penile rash, knee swelling, tongue changes, red eyes, and low back pain. He had had diarrhea and urethral discharge 7 days before the onset of symptoms. On examination, yellow pustules with hyperkeratosis were seen on his plantar feet. What is the name of this physical examination sign?
1. Keratoderma blennorrhagicum
2. Palmoplantar keratoderma
3. Pitted keratolysis
4. Porokeratosis
5. Pustular psoriasis
1. Keratoderma blennorrhagicum
2. Palmoplantar keratoderma
3. Pitted keratolysis
4. Porokeratosis
5. Pustular psoriasis
Answer: 1. Keratoderma blennorrhagicum
This patient has reactive arthritis (previously known as Reiter disease), which is a syndrome consisting of urethritis, arthritis, ocular findings and oral ulcers, in addition to psoriasiform lesions. Chlamydia trachomatis is one of the major causes of the urethritis and may trigger the entire syndrome (although this patient tested negative for all infectious agents). Polyarthritis and /sacroiliitis are the most common joint manifestations. Keratoderma blennorrhagicum refers to lesions on the plantar surface that usually have a thick yellow scale and are often pustular. The patient also had new psoriatic skin lesions on scalp, trunk and dorsal hands in addition to pitting and distal onycholysis on some nails. Psoriatic plaques on the penis are known as balanitis circinata. Reactive arthritis has a strong association with HLA-B27, for which this patient was positive.
Other answers:
2. Palmoplantar keratoderma: this refers to a wide group of inherited or acquired disorders that present with hyperkeratosis of palmar and/or plantar skin. The pustular lesions with hyperkeratosis in the setting of reactive arthritis makes keratoderma blennorrhagicum the correct answer
3. Pitted keratolysis: this is caused by a gram-positive bacteria called Kytococcus sedentarius, which digests keratin in stratum corneum. It presents with small crateriform pits and foul order
4. Porokeratosis: there are at least 6 clinical variants with some of the variants having lesions on the palms/soles. Porokeratosis palmaris et plantaris disseminata (PPD) is one of the variants which presents with palmoplantar papules in addition to involvement of the trunk, extremities and even other body parts. Punctate porokeratosis presents with palmoplantar papules that measure 1-2 mm in diameter
5. Pustular psoriasis: generalized pustular psoriasis can present with two forms 1) impetigo herpetiformis which is pregnancy-associated and 2) von Zumbusch which presents with painful skin, fever, leukocytosis, hypoalbuminemia (the patient is very sick). Palmoplantar pustulosis is a variant of psoriasis that presents with pustules and yellow-brown macules localized to palms/soles
Explanations developed with use of Alikhan, Ali, and Thomas LH Hocker. Review of Dermatology E-Book. Elsevier Health Sciences, 2017.
This patient has reactive arthritis (previously known as Reiter disease), which is a syndrome consisting of urethritis, arthritis, ocular findings and oral ulcers, in addition to psoriasiform lesions. Chlamydia trachomatis is one of the major causes of the urethritis and may trigger the entire syndrome (although this patient tested negative for all infectious agents). Polyarthritis and /sacroiliitis are the most common joint manifestations. Keratoderma blennorrhagicum refers to lesions on the plantar surface that usually have a thick yellow scale and are often pustular. The patient also had new psoriatic skin lesions on scalp, trunk and dorsal hands in addition to pitting and distal onycholysis on some nails. Psoriatic plaques on the penis are known as balanitis circinata. Reactive arthritis has a strong association with HLA-B27, for which this patient was positive.
Other answers:
2. Palmoplantar keratoderma: this refers to a wide group of inherited or acquired disorders that present with hyperkeratosis of palmar and/or plantar skin. The pustular lesions with hyperkeratosis in the setting of reactive arthritis makes keratoderma blennorrhagicum the correct answer
3. Pitted keratolysis: this is caused by a gram-positive bacteria called Kytococcus sedentarius, which digests keratin in stratum corneum. It presents with small crateriform pits and foul order
4. Porokeratosis: there are at least 6 clinical variants with some of the variants having lesions on the palms/soles. Porokeratosis palmaris et plantaris disseminata (PPD) is one of the variants which presents with palmoplantar papules in addition to involvement of the trunk, extremities and even other body parts. Punctate porokeratosis presents with palmoplantar papules that measure 1-2 mm in diameter
5. Pustular psoriasis: generalized pustular psoriasis can present with two forms 1) impetigo herpetiformis which is pregnancy-associated and 2) von Zumbusch which presents with painful skin, fever, leukocytosis, hypoalbuminemia (the patient is very sick). Palmoplantar pustulosis is a variant of psoriasis that presents with pustules and yellow-brown macules localized to palms/soles
Explanations developed with use of Alikhan, Ali, and Thomas LH Hocker. Review of Dermatology E-Book. Elsevier Health Sciences, 2017.
SK(IN DEPTH) RECAP
1. In the meta-analysis by Bailey et al., what were potential side effects of microneedling for treatment of melasma?
A. Transient burning
B. Itching
C. Erythema
D. Changes in pigmentation
E. All of the above
2. In Mulder et al., what are inflammatory changes seen within a week of burn injury in an animal model?
A. Increased neutrophils, increased monocytes, increased thrombocytes
B. Increased neutrophils, decreased monocytes, decreased lymphocytes
C. Decreased neutrophils, increased monocytes, increased thrombocytes
D. Decreased neutrophils, decreased monocytes, decreased lymphocytes
A. Transient burning
B. Itching
C. Erythema
D. Changes in pigmentation
E. All of the above
2. In Mulder et al., what are inflammatory changes seen within a week of burn injury in an animal model?
A. Increased neutrophils, increased monocytes, increased thrombocytes
B. Increased neutrophils, decreased monocytes, decreased lymphocytes
C. Decreased neutrophils, increased monocytes, increased thrombocytes
D. Decreased neutrophils, decreased monocytes, decreased lymphocytes
1. In the meta-analysis by Bailey et al., what were potential side effects of microneedling for treatment of melasma?
A. Transient burning
B. Itching
C. Erythema
D. Changes in pigmentation
E. All of the above
All of the above! Overall, microneedling was well-tolerated without serious adverse effects. However, be on the lookout for transient burning, itching, erythema, and dyspigmentation reported by patients.
2. In Mulder et al., what are inflammatory changes seen within a week of burn injury in an animal model?
A. Increased neutrophils, increased monocytes, increased thrombocytes
B. Increased neutrophils, decreased monocytes, decreased lymphocytes
C. Decreased neutrophils, increased monocytes, increased thrombocytes
D. Decreased neutrophils, decreased monocytes, decreased lymphocytes
In the first week post-burn, the authors found increased numbers of neutrophils, monocytes, and thrombocytes in the peripheral blood, which remained high for up to a month after the injury. In addition to detailing other temporal immune cell dynamics, the authors conclude that burn injury likely results in long-lasting inflammatory changes.
A. Transient burning
B. Itching
C. Erythema
D. Changes in pigmentation
E. All of the above
All of the above! Overall, microneedling was well-tolerated without serious adverse effects. However, be on the lookout for transient burning, itching, erythema, and dyspigmentation reported by patients.
2. In Mulder et al., what are inflammatory changes seen within a week of burn injury in an animal model?
A. Increased neutrophils, increased monocytes, increased thrombocytes
B. Increased neutrophils, decreased monocytes, decreased lymphocytes
C. Decreased neutrophils, increased monocytes, increased thrombocytes
D. Decreased neutrophils, decreased monocytes, decreased lymphocytes
In the first week post-burn, the authors found increased numbers of neutrophils, monocytes, and thrombocytes in the peripheral blood, which remained high for up to a month after the injury. In addition to detailing other temporal immune cell dynamics, the authors conclude that burn injury likely results in long-lasting inflammatory changes.