Fifty-Third issue
February 7, 2024
Short-term cardiovascular complications in dermatology patients receiving JAK-STAT inhibitors: A meta-analysis of randomized clinical trials
JAMA Dermatology
JAMA Dermatology
JAK up your heart health!
The ORAL study suggested that JAK-STAT inhibitor use in patients with rheumatoid arthritis may pose a greater risk for major adverse cardiovascular events (MACE) and venous thromboembolism (VTE), causing the implementation of a classwide black box warning.
This systematic review and meta-analysis aimed to determine if JAK-STAT inhibitor use for common dermatoses also increases risk for MACE and VTE. 45 randomized clinical trials assessed 12,996 patients receiving JAK-STAT inhibitor therapy and 4,925 patients receiving placebo treatment for alopecia areata, psoriasis, vitiligo, atopic dermatitis, lichen planus, or hidradenitis suppurativa.
What did they find?
Limitations: Studies included had short follow-ups, limiting insight for extended use of JAK-STAT inhibitors. Studies did not control for known MACE and VTE risk factors.
Main Takeaway: Using JAK-STAT inhibitors in short intervals in patients with dermatologic indications and low cardiovascular risk profiles was not associated with an increased risk of MACE or VTE.
The ORAL study suggested that JAK-STAT inhibitor use in patients with rheumatoid arthritis may pose a greater risk for major adverse cardiovascular events (MACE) and venous thromboembolism (VTE), causing the implementation of a classwide black box warning.
This systematic review and meta-analysis aimed to determine if JAK-STAT inhibitor use for common dermatoses also increases risk for MACE and VTE. 45 randomized clinical trials assessed 12,996 patients receiving JAK-STAT inhibitor therapy and 4,925 patients receiving placebo treatment for alopecia areata, psoriasis, vitiligo, atopic dermatitis, lichen planus, or hidradenitis suppurativa.
What did they find?
- No significant increase in MACE (I2 = 0.00%; RR, 0.47; 95% CI, 0.28-0.80) or VTE (I2 = 0.00%; RR, 0.46; 95% CI, 0.26-0.80) in patients who were treated with JAK-STAT inhibitors compared to placebo with a median duration of 16 weeks
- No significant increase in serious adverse events (I2 = 12.38%; RR, 0.92; 95% CI, 0.72-1.20) or medication discontinuations (I2 = 23.55%; RR, 0.94; 95% CI, 0.76-1.19) for patients using JAK-STAT inhibitors compared to placebo
Limitations: Studies included had short follow-ups, limiting insight for extended use of JAK-STAT inhibitors. Studies did not control for known MACE and VTE risk factors.
Main Takeaway: Using JAK-STAT inhibitors in short intervals in patients with dermatologic indications and low cardiovascular risk profiles was not associated with an increased risk of MACE or VTE.
Best practices in the treatment of melasma with a focus on patients with skin of color
Journal of American Academy Dermatology
Journal of American Academy Dermatology
Melasma? More like me-LAST-ma: The ultimate guide to putting an end to melasma
Melasma is a chronic hypermelanosis of the skin that predominantly affects women with skin of color or those who are pregnant. Typically manifesting as symmetric hyperpigmentation in sun-exposed areas, melasma has a complex pathogenesis with no current cure. While a variety of treatment options exist, a general consensus on how to best manage the condition is lacking. This best practice guide strives to set forth an outline and stepwise approach to treating patients with melasma.
2. Triple-Combination Cream (TCC) of 4% Hydroquinone (HQ), 0.05% Tretinoin, and 0.01% Fluocinolone Acetonide
3. Oral Tranexamic Acid (TA)
4. Alternative Therapies
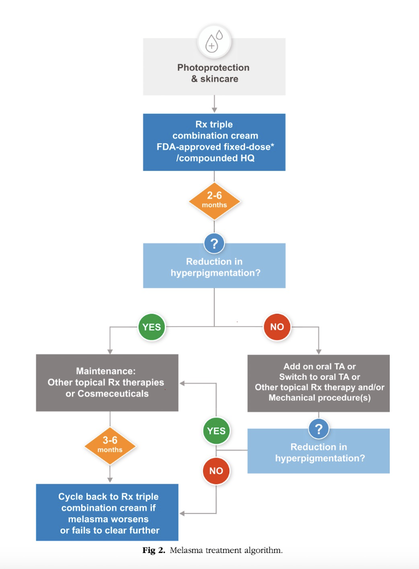
The algorithm below provides recommendations for cycling treatment therapies over a period of time based upon patient response.
Melasma is a chronic hypermelanosis of the skin that predominantly affects women with skin of color or those who are pregnant. Typically manifesting as symmetric hyperpigmentation in sun-exposed areas, melasma has a complex pathogenesis with no current cure. While a variety of treatment options exist, a general consensus on how to best manage the condition is lacking. This best practice guide strives to set forth an outline and stepwise approach to treating patients with melasma.
- Photoprotection/Skin Care
- UV radiation is a major driver in melasma pathogenesis
- Photoprotective measures (sunscreen and sun protective clothing) should be first-line in melasma control
- Consistent skincare, including gentle cleansers and moisturizers, are important interventions as they help to restore skin barrier function and increase cell turnover
2. Triple-Combination Cream (TCC) of 4% Hydroquinone (HQ), 0.05% Tretinoin, and 0.01% Fluocinolone Acetonide
- FDA-approved fixed-dose TCC is also considered first-line treatment with proven safety and efficacy in usage for up to 6 month
3. Oral Tranexamic Acid (TA)
- In non-responders or those unable to tolerate topical treatments, oral tranexamic acid, a plasmin inhibitor which leads to a decrease in melanogenic factors, has shown to exhibit similar efficacy
4. Alternative Therapies
- Vitamin C, kojic acid, niacinamide, and azelaic acid are popular natural compounds proposed to target melanogenesis
- Of note, no studies show improved efficacy of these compounds compared to TCC
- Mechanical or energy-based procedures can be helpful adjuvants, but should not be considered first-line
The algorithm below provides recommendations for cycling treatment therapies over a period of time based upon patient response.
Lastly, it is crucial that patients understand melasma is a chronic condition, and prevention of flairs is a long-term commitment, often requiring continuous maintenance treatment.
Main takeaway: Melasma can be challenging to treat. However, this best practice guide lays forth an outline of effective treatment options including photoprotection, triple-combination cream, and tranexamic acid.
Main takeaway: Melasma can be challenging to treat. However, this best practice guide lays forth an outline of effective treatment options including photoprotection, triple-combination cream, and tranexamic acid.
Selective depletion of S. aureus restores the skin microbiome and accelerates tissue repair following injury
Journal of Investigative Dermatology
Journal of Investigative Dermatology
XZ.700: an enticin’ endolysin
Staphylococcus aureus skin infections cause microbial dysbiosis and barrier perturbation, leading to delayed wound healing following injury. Endolysins are bacterial-derived cell wall lytic enzymes that can degrade peptidoglycan in gram-positive bacteria. Because S. aureus exhibits high levels of antimicrobial resistance, researchers sought to evaluate the selectivity and efficacy of treatment of S. aureus infected wounds with a targeted endolysin, XZ.700.
Researchers induced injury in ex-vivo porcine skin models (N=3) and S. aureus colonization was measured over time. Samples were treated with XZ.700 and changes in the skin microbiome and wound healing were compared to control.
What did they find?
Main Takeaways: XZ.700 is associated with improved wound healing and amelioration of dysbiosis in S. aureus skin infection, making it a potential targeted treatment option.
Staphylococcus aureus skin infections cause microbial dysbiosis and barrier perturbation, leading to delayed wound healing following injury. Endolysins are bacterial-derived cell wall lytic enzymes that can degrade peptidoglycan in gram-positive bacteria. Because S. aureus exhibits high levels of antimicrobial resistance, researchers sought to evaluate the selectivity and efficacy of treatment of S. aureus infected wounds with a targeted endolysin, XZ.700.
Researchers induced injury in ex-vivo porcine skin models (N=3) and S. aureus colonization was measured over time. Samples were treated with XZ.700 and changes in the skin microbiome and wound healing were compared to control.
What did they find?
- XZ.700 significantly reduced the growth of methicillin-susceptible S. aureus (P<0.001) and methicillin-resistant S. aureus (P<0.001) in human wound isolated biofilms
- There was no effect on S. epidermidis when co-cultured with MRSA (P<0.001), establishing its selectivity for S. aureus
- There was no effect on S. epidermidis when co-cultured with MRSA (P<0.001), establishing its selectivity for S. aureus
- XZ.700-treated porcine skin models harbored significantly less S. aureus compared to control over 16 days (P<0.001), showing potent antimicrobial effects
- The alpha diversity of the skin microbiome was significantly reduced in porcine skin wounds following injury (P<0.001), and treatment with XZ.700 increased alpha diversity in wound on day 4 post-injury (P<0.05)
- On day 16 post-injury, XZ.700-treated porcine skin models displayed reduced wound width (P<0.05), granulation tissue area (P<0.01), number of infiltrating macrophages (P<0.05), and increased collagen deposition (P<0.05) compared to control
Main Takeaways: XZ.700 is associated with improved wound healing and amelioration of dysbiosis in S. aureus skin infection, making it a potential targeted treatment option.
Is precision cryotherapy an effective treatment of seborrheic dermatitis of the scalp?
Dermatologic Surgery
Dermatologic Surgery
Seborrheic dermatitis itch? Don’t cry, try precision cryotherapy!
Seborrheic dermatitis (SD) causes pruritic, scaly patches on the scalp. While current treatments are effective, many patients relapse after discontinuing treatment. Novel precision cryotherapy (PC) devices precisely control skin surface temperature to as cool as 1 ℃. This single-arm, open label prospective clinical trial evaluated the anti-inflammatory and antipruritic effects of PC in patients with scalp SD.
Participants (n = 22) underwent 3 PC treatments q2 weeks. Pruritus (visual analog scale), physician global assessment, clinical severity scores, erythema, and transepidermal water loss were measured at baseline, 6 weeks, and 8 weeks.
What did they find?
Main Takeaways: Patients with scalp SD had improved severity scores, physician assessment scores, erythema index, and pruritic symptoms after 3 treatments of precision cryotherapy.
Seborrheic dermatitis (SD) causes pruritic, scaly patches on the scalp. While current treatments are effective, many patients relapse after discontinuing treatment. Novel precision cryotherapy (PC) devices precisely control skin surface temperature to as cool as 1 ℃. This single-arm, open label prospective clinical trial evaluated the anti-inflammatory and antipruritic effects of PC in patients with scalp SD.
Participants (n = 22) underwent 3 PC treatments q2 weeks. Pruritus (visual analog scale), physician global assessment, clinical severity scores, erythema, and transepidermal water loss were measured at baseline, 6 weeks, and 8 weeks.
What did they find?
- Pruritic symptoms declined by 50.4% at 8 weeks post-treatment compared to baseline
- 6.77 土 2.29 at baseline vs. 3.36 土 2.46 at Week 8 (p = <.01)
- 6.77 土 2.29 at baseline vs. 3.36 土 2.46 at Week 8 (p = <.01)
- Physician global assessment scores improved from a mean of 2.86 土 0.62 at baseline to 1.66 土 0.61 at Week 8
- Clinical severity scores decreased 46.2% from baseline to Week 8
- The mean erythema index declined 19.6% from baseline to Week 8 (p= .05)
- Transepidermal water loss showed a decreasing but not statistically significant trend from baseline to Week 8
Main Takeaways: Patients with scalp SD had improved severity scores, physician assessment scores, erythema index, and pruritic symptoms after 3 treatments of precision cryotherapy.
How effective is multicorrective topical treatment for infraorbital dark circles and puffiness?
Journal of Cosmetic Dermatology
Journal of Cosmetic Dermatology
Let’s put away the eye bags for good!
The pathogenesis of infraorbital dark circles and puffiness involves microvasculature congestion, melanin build up, and pigment deposition from hemoglobin degradation. Despite various therapeutics, individuals often experience suboptimal results.
This study evaluates the effectiveness and tolerance of a multicorrective topical eye cream (MTEC) containing tetrahexyldecyl ascorbate, prebiotics, three bioavailable peptides, botanical extracts (Jasminum sambac, and Crataegus monogyna), chrysin, and caffeine.
Women (n=37) with moderate-to-severe infraorbital dark marks with puffiness applied MTEC to the affected area twice daily for 12 weeks. Patients were clinically evaluated at baseline, 4, 8, and 12 weeks for infraorbital dark circles, under-eye puffiness, and overall appearance.
What did they find:
Main takeaway: A novel multicorrective topical eye cream successfully diminished under-eye dark circles and puffiness with favorable tolerability. Additionally, it demonstrated reduction in vascular features and improved redness associated with under-eye dark circles.
The pathogenesis of infraorbital dark circles and puffiness involves microvasculature congestion, melanin build up, and pigment deposition from hemoglobin degradation. Despite various therapeutics, individuals often experience suboptimal results.
This study evaluates the effectiveness and tolerance of a multicorrective topical eye cream (MTEC) containing tetrahexyldecyl ascorbate, prebiotics, three bioavailable peptides, botanical extracts (Jasminum sambac, and Crataegus monogyna), chrysin, and caffeine.
Women (n=37) with moderate-to-severe infraorbital dark marks with puffiness applied MTEC to the affected area twice daily for 12 weeks. Patients were clinically evaluated at baseline, 4, 8, and 12 weeks for infraorbital dark circles, under-eye puffiness, and overall appearance.
What did they find:
- Under-eye dark circles significantly improved by 12.5%, 20%, and 20% after weeks 4, 8, and 12, respectively, compared to baseline (p<0.001)
- Overall eye appearance improved by 14.3% after 12 weeks of treatment (p<0.01)
- A 16.7% improvement in under-eye puffiness was observed at week 8 and week 12 (p<0.001)
- Photo analysis indicated up to 17% reduction in under-eye dark circle redness and brown pigmentation at week 12 compared to baseline
- Dryness was reported by two participants, and it resolved by week 12. There were no instances of edema, stinging, tingling, itching, or burning reported throughout the study
Main takeaway: A novel multicorrective topical eye cream successfully diminished under-eye dark circles and puffiness with favorable tolerability. Additionally, it demonstrated reduction in vascular features and improved redness associated with under-eye dark circles.
Effect of Shikonin Treatment on B16F10 Melanoma Cells
While early-stage melanoma is treatable with surgery, advanced melanoma often resists chemotherapy due to apoptosis evasion. Shikonin-induced necroptosis offers an innovative, resistance-free pathway for melanoma treatment; this approach may overcome current therapy limitations, offering new options for advanced melanoma patients.
B16F10 melanoma cell growth with shikonin was analyzed using MTT assay. Shikonin, combined with either necrostatin, caspase inhibitor, 3-methyladenine, or N-acetyl cysteine, was examined. Flow cytometry assessed cell death types. BrdU labeling analyzed cell proliferation. Monodansylcadaverine staining gauged autophagy levels. Western blot identified CHOP, RIP1, and pRIP1. MitoTracker staining revealed mitochondrial density differences in shikonin-treated cells.
What did we find?
Main takeaway: Our findings suggest that mainly necroptosis is induced by shikonin treatment of B16F10 melanoma cells. Induction of autophagy and ROS production are also involved.
B16F10 melanoma cell growth with shikonin was analyzed using MTT assay. Shikonin, combined with either necrostatin, caspase inhibitor, 3-methyladenine, or N-acetyl cysteine, was examined. Flow cytometry assessed cell death types. BrdU labeling analyzed cell proliferation. Monodansylcadaverine staining gauged autophagy levels. Western blot identified CHOP, RIP1, and pRIP1. MitoTracker staining revealed mitochondrial density differences in shikonin-treated cells.
What did we find?
- Analysis of MTT assays revealed a large decrease in cellular growth with increasing shikonin concentrations
- The MTT assays with necrostatin, 3-methyladenine, and N-acetyl cysteine involvement suggested that necroptosis, autophagy, and reactive oxygen species are a part of shikonin’s mechanism of action
- Cellular proliferation with shikonin treatment was also decreased
- Western blotting confirmed upregulation of stress related proteins
Main takeaway: Our findings suggest that mainly necroptosis is induced by shikonin treatment of B16F10 melanoma cells. Induction of autophagy and ROS production are also involved.