Forty-sixth ISSUE
November 1, 2023
Is there an increased risk of IBD, UC, and CD in children and adults with atopic dermatitis?
JAMA Dermatology
JAMA Dermatology
Haven’t you heard? The HPA is old news…we’re all about the gut-brain-skin axis these days!
Context/background and methods:
Atopic dermatitis (AD) and inflammatory bowel disease (IBD) are two common inflammatory conditions with some overlapping treatment modalities. Few studies have evaluated the association and severity of AD with the risk of ulcerative colitis (UC) and Crohn’s disease (CD). This population-based cohort study (n=409,431 children and n=625,083 adults) investigated the incidence of IBD in patients with AD. Severity of AD was evaluated through examining treatment modality.
What did they find?
Limitations: Treatment modalities were used as an indication of severity of AD and surveillance bias could have been a factor as patients with more severe AD were followed more closely.
Main Takeaway: There is an increased risk of new-onset IBD in children and adults with AD. It is necessary to be aware of these risks, especially when selecting systemic treatments for these patients.
Context/background and methods:
Atopic dermatitis (AD) and inflammatory bowel disease (IBD) are two common inflammatory conditions with some overlapping treatment modalities. Few studies have evaluated the association and severity of AD with the risk of ulcerative colitis (UC) and Crohn’s disease (CD). This population-based cohort study (n=409,431 children and n=625,083 adults) investigated the incidence of IBD in patients with AD. Severity of AD was evaluated through examining treatment modality.
What did they find?
- Children with AD had:
- 44% increased risk of IBD (HR 1.44, 95% CI, 1.31-1.58)
- 74% increased risk of CD
- no increased risk of UC (HR 1.09, 95% CI, 0.94-1.27) unless they had severe AD (HR 1.65, 95% CI, 1.02-2.67)
- 44% increased risk of IBD (HR 1.44, 95% CI, 1.31-1.58)
- Adults with AD had:
- 34% increased risk of IBD (HR 1.34, 95% CI, 1.27-1.40)
- 36% increased risk of CD (HR 1.36, 95% CI, 1.26-1.47)
- 32% increased risk of UC (HR 1.32, 95% CI, 1.24-1.41)
- 34% increased risk of IBD (HR 1.34, 95% CI, 1.27-1.40)
- Risk of IBD, UC, and CD in both adults and children increased with increasing severity of AD
Limitations: Treatment modalities were used as an indication of severity of AD and surveillance bias could have been a factor as patients with more severe AD were followed more closely.
Main Takeaway: There is an increased risk of new-onset IBD in children and adults with AD. It is necessary to be aware of these risks, especially when selecting systemic treatments for these patients.
Efficacy and safety of clindamycin phosphate 1.2%/adapalene 0.15%/benzoyl peroxide 3.1% gel for moderate-to-severe acne
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Triple therapy, triple threat!
Acne is a common skin condition caused by abnormal keratinization, increased inflammation and sebum production, and the proliferation of Cutibactrium acnes. Commonly used topical treatments for acne include clindamycin, benzoyl peroxide (BPO), and adapalene. There is growing interest in a fixed-dose triple combination therapy, which may provide better efficacy than mono- or dual therapy and improve patient adherence.
This study included two phase 3, double-blind, 12-week randomized control trials (n = 183; n = 180). Patients ≥ 9 years old with moderate to severe acne were randomized 2:1 to receive once-daily topical clindamycin phosphate 1.2%/adapalene 0.15%/BPO 3.1% gel (IDP-126) or vehicle gel.
What did they find?
Main Takeaways: Once-daily treatment with fixed-dose triple-combination clindamycin phosphate 1.2%/adapalene 0.15%/BPO 3.1% gel demonstrated efficacy and safety and is a potential new treatment for patients with moderate to severe acne.
Acne is a common skin condition caused by abnormal keratinization, increased inflammation and sebum production, and the proliferation of Cutibactrium acnes. Commonly used topical treatments for acne include clindamycin, benzoyl peroxide (BPO), and adapalene. There is growing interest in a fixed-dose triple combination therapy, which may provide better efficacy than mono- or dual therapy and improve patient adherence.
This study included two phase 3, double-blind, 12-week randomized control trials (n = 183; n = 180). Patients ≥ 9 years old with moderate to severe acne were randomized 2:1 to receive once-daily topical clindamycin phosphate 1.2%/adapalene 0.15%/BPO 3.1% gel (IDP-126) or vehicle gel.
What did they find?
- At week 12, 49.6% and 50.5% of participants achieved treatment success with IDP-126 versus 24.9% and 20.5% with vehicle in studies 1 and 2, respectively (P < 0.01, both)
- Absolute mean reductions in inflammatory and noninflammatory lesions from baseline to week 12 were significantly greater with IDP-126 versus vehicle (P < 0.001, both)
- More participants achieved a 2-grade reduction in EGSS at week 12 with IDP-126 versus vehicle (P < 0.001)
- More participants in the IDP-126 group reported treatment-emergent adverse events, most commonly erythema, application-site pain, dryness, irritation, and exfoliation
Main Takeaways: Once-daily treatment with fixed-dose triple-combination clindamycin phosphate 1.2%/adapalene 0.15%/BPO 3.1% gel demonstrated efficacy and safety and is a potential new treatment for patients with moderate to severe acne.
What are the clinical features and course of atypical hand-foot-mouth disease in children?
Pediatric Dermatology
Pediatric Dermatology
Why is hand, foot, and mouth disease everywhere in schools? Because it wanted to get a real "hands-on" education!
Hand-foot-mouth disease (HFMD) is a common childhood infection caused by enteroviruses. While classically presenting as painful, erythematous macules/papules/ulcers, atypically presenting HFMD may resemble eczema herpeticum, Gianotti-Crosti disease, or Stevens-Johnson syndrome.
Atypical presentations of HFMD usually have greater body distribution and are accompanied by systemic symptoms such as fever and oropharyngeal pain, which may lead to higher hospital admission rates. To better characterize the clinical characteristics of atypical HFMD, researchers conducted a systematic review of 85 studies comprising 1359 pediatric patients between the ages of 19 days and 18 years.
What did they find?
Limitation: This study is limited by minimal follow-up leading to incomplete reporting of complications, and a possible overrepresentation of severe or unusual cases due to publication bias.
Main Takeaways: The diagnosis of atypical HFMD is frequently overlooked due to its diverse clinical appearance, often resembling other skin conditions, and this study aimed to highlight atypical manifestations to enable early recognition.
Hand-foot-mouth disease (HFMD) is a common childhood infection caused by enteroviruses. While classically presenting as painful, erythematous macules/papules/ulcers, atypically presenting HFMD may resemble eczema herpeticum, Gianotti-Crosti disease, or Stevens-Johnson syndrome.
Atypical presentations of HFMD usually have greater body distribution and are accompanied by systemic symptoms such as fever and oropharyngeal pain, which may lead to higher hospital admission rates. To better characterize the clinical characteristics of atypical HFMD, researchers conducted a systematic review of 85 studies comprising 1359 pediatric patients between the ages of 19 days and 18 years.
What did they find?
- Atypical skin manifestations of HFMD showed male predominance (61%, 387/635) with a mean age of 2.4 years and symptom duration of 10 days
- Baseline dermatological conditions were reported in 109 out of 1359 cases, the most common being atopic dermatitis (93/109)
- The most common atypical lesion sites were arms and/or legs (47%), face (45%), and buttocks (28%)
- Extracutaneous manifestations included fever (74%), pharyngitis (18%), and cough (16%)
- 40% of cases required hospitalization (40%), and common complications after the cutaneous rash phase included nail changes (21%) and desquamation (4%)
Limitation: This study is limited by minimal follow-up leading to incomplete reporting of complications, and a possible overrepresentation of severe or unusual cases due to publication bias.
Main Takeaways: The diagnosis of atypical HFMD is frequently overlooked due to its diverse clinical appearance, often resembling other skin conditions, and this study aimed to highlight atypical manifestations to enable early recognition.
Exploring the natural and treatment history of vitiligo: perceptions of patients and healthcare professionals from the global VALIANT study
British Journal of Dermatology
British Journal of Dermatology
VITI–whyyyyyy don’t we have better treatments--GO
Vitiligo is an autoimmune condition that affects up to 2% of the world population; it is characterized by patches of depigmented skin. Vitiligo can have a significant impact on quality of life, but patients often report feeling that these concerns are dismissed as a largely cosmetic condition. To date, there are relatively few available therapies for vitiligo. To better understand the natural history and clinical management of vitiligo worldwide, researchers performed a cross-sectional observational survey of patients and healthcare professionals from 17 countries.
What did they find?
Main takeaways: Although vitiligo affects many people worldwide, many patients are frustrated at the lack of effective therapeutic options. These data emphasize the importance of identifying new and accessible therapies for vitiligo.
Limitations: This is a survey-based study, so data is subject to recall biases. This was an internet-based survey, which may lead to selection bias and over/underrepresentation of certain patient groups.
Vitiligo is an autoimmune condition that affects up to 2% of the world population; it is characterized by patches of depigmented skin. Vitiligo can have a significant impact on quality of life, but patients often report feeling that these concerns are dismissed as a largely cosmetic condition. To date, there are relatively few available therapies for vitiligo. To better understand the natural history and clinical management of vitiligo worldwide, researchers performed a cross-sectional observational survey of patients and healthcare professionals from 17 countries.
What did they find?
- Nearly half of patients (45%) had >5% affected body surface area
- 57% reported a family history of vitiligo
- Mean time to diagnosis was 2.4 years; 45% of patients had been previously misdiagnosed
- 57% were told vitiligo could not be treated and 26% did not believe in an effective therapy
- Patient priorities included:
- reduction or cessation of spread
- re-pigmentation
Main takeaways: Although vitiligo affects many people worldwide, many patients are frustrated at the lack of effective therapeutic options. These data emphasize the importance of identifying new and accessible therapies for vitiligo.
Limitations: This is a survey-based study, so data is subject to recall biases. This was an internet-based survey, which may lead to selection bias and over/underrepresentation of certain patient groups.
Be Comfortable in Your Own “e-skin”
E-skin (or second skin) are sensors that cover a wide area of skin that protect the stratum corneum from environmental factors with data processing capabilities. Functions of e-skins may range from temperature and pressure sensors, currents to stimulate wound healing, anti-microbial barriers and pathogen detection, and ability to stimulate receptors on the surface of the skin that could incite the release of oxytocin via mimicking human touch.
What do they do?
E-skin (or second skin) are sensors that cover a wide area of skin that protect the stratum corneum from environmental factors with data processing capabilities. Functions of e-skins may range from temperature and pressure sensors, currents to stimulate wound healing, anti-microbial barriers and pathogen detection, and ability to stimulate receptors on the surface of the skin that could incite the release of oxytocin via mimicking human touch.
What do they do?
- E-skins can generate electromagnetic waves to keratinocytes affecting their multitude of receptors
- E-skins can active opsin receptors leading to skin melanization, photoaging, regulation of the biological clock and epidermal proliferation
- There is exploration using E-Skin to activate TRP in keratinocytes for epidermal differentiation and skin barrier for pathogen detection
- E-skins can use electrical potential to increase keratinocyte migration and increase wound healing
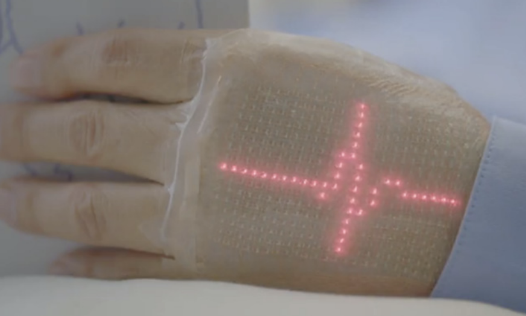
Figure 1. “An ultrathin, elastic display that fits snugly on the skin shows the moving waveform of an electrocardiogram. This image is courtesy of the University of Tokyo and DNP in an academic-industrial collaboration. DNP, Dai Nippon Printing.”
Main Takeaway: E-skins are newly advancing technology in the field of medicine that can function in a variety of ways from wound healing to temperature and pressure sensing and pathogen detection.
Limitation: The biological effects of e-skins are not entirely understood so further research is warranted to better understand their implications on sensors within the skin.
Main Takeaway: E-skins are newly advancing technology in the field of medicine that can function in a variety of ways from wound healing to temperature and pressure sensing and pathogen detection.
Limitation: The biological effects of e-skins are not entirely understood so further research is warranted to better understand their implications on sensors within the skin.
Skin of color photo representation in case reports has increased but lacks standardization
JMIR Dermatology
JMIR Dermatology
Intro: Our study assessed skin of color (SoC) representation and race/ethnicity reporting in all case photos published by JAAD Case Reports from 2015 through 2021. We investigated this topic to discuss the underrepresentation of SoC in academic resources and to identify trends in JAAD publishing.
Methods: A total of 2451 case report photos were assessed by two independent blinded reviewers and recorded as either light (Fitzpatrick I-II), medium (III-IV), or dark (V-VI). A third reviewer resolved discrepancies prior to analysis. Author-reported race/ethnicity was included for analysis.
Results:
Limitations: Photos taken of the subjects did not have standard lighting or quality, which could have impacted the viewer’s perception of true skin tone.
Conclusions: While the publishing of SoC cases increased over the years, we encourage academic resources to continue improving these rates and to standardize reporting of race/ethnicity. Case reports can help physicians recognize and treat novel occurrences and can lead to advancements in research and clinical practice. Thus, it’s essential that they represent a diverse population to improve clinical care for all patients.
Reflection: This was our first experience formally analyzing a large data set and we learned the importance of planning and standardizing the data collection prior to getting started.
Methods: A total of 2451 case report photos were assessed by two independent blinded reviewers and recorded as either light (Fitzpatrick I-II), medium (III-IV), or dark (V-VI). A third reviewer resolved discrepancies prior to analysis. Author-reported race/ethnicity was included for analysis.
Results:
- Images perceived as light decreased from 73% in 2015 to 59% in 2021, corresponding with increased percentages of medium and dark skin tones perceived
- Race/ethnicity reporting decreased from 40% in 2015 to 24% in 2021
- 65% of cases that did not include an image were reported as White
Limitations: Photos taken of the subjects did not have standard lighting or quality, which could have impacted the viewer’s perception of true skin tone.
Conclusions: While the publishing of SoC cases increased over the years, we encourage academic resources to continue improving these rates and to standardize reporting of race/ethnicity. Case reports can help physicians recognize and treat novel occurrences and can lead to advancements in research and clinical practice. Thus, it’s essential that they represent a diverse population to improve clinical care for all patients.
Reflection: This was our first experience formally analyzing a large data set and we learned the importance of planning and standardizing the data collection prior to getting started.