SEVENTEENTH ISSUE
August 24, 2022
How much prior knowledge is too much knowledge?
In medicine, we frequently consult our colleagues, especially when evaluating a complex case. It is important to be aware of anchoring bias, which is when a second opinion is swayed by the preliminary diagnosis. This study sought to determine if dermatopathologists who are consulted for second opinions are affected by anchoring bias.
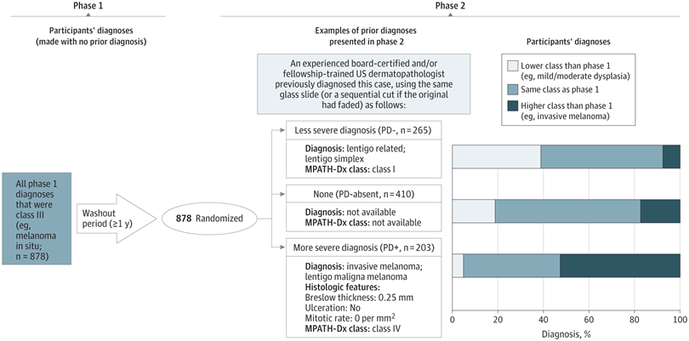
Focusing on melanocytic lesions, 90 cases were selected, and consensus diagnoses were performed by expert dermatopathologists. In phase 1 of this study, 149 dermatopathologists evaluated histopathologic slides. After a one-year washout period, those dermatopathologists re-evaluated the same slides as they did during phase 1. However, this time they were provided a diagnosis from a third-party “consulting”physician beforehand; some of these preliminary diagnoses were the true diagnosis, while others were purposefully provided either less or more severe preliminary diagnoses. The influence of this knowledge was evaluated.
In medicine, we frequently consult our colleagues, especially when evaluating a complex case. It is important to be aware of anchoring bias, which is when a second opinion is swayed by the preliminary diagnosis. This study sought to determine if dermatopathologists who are consulted for second opinions are affected by anchoring bias.
Focusing on melanocytic lesions, 90 cases were selected, and consensus diagnoses were performed by expert dermatopathologists. In phase 1 of this study, 149 dermatopathologists evaluated histopathologic slides. After a one-year washout period, those dermatopathologists re-evaluated the same slides as they did during phase 1. However, this time they were provided a diagnosis from a third-party “consulting”physician beforehand; some of these preliminary diagnoses were the true diagnosis, while others were purposefully provided either less or more severe preliminary diagnoses. The influence of this knowledge was evaluated.
Using the Melanocytic Pathology Assessment Tool and Hierarchy for Diagnoses, Stage III lesions (which includes melanoma in-situ and atypical spitz nevi) were investigated. 39% of dermatopathologists made a lower-grade diagnosis during Phase 2 when the “consulting” dermatopathologist made a less severe preliminary diagnosis (odds ratio 1.38, confidence interval 1.19-1.59). When provided a more severe prior diagnosis from the “consulting” physician, 53% of dermatopathologists subsequently made a higher-grade diagnosis (odds ratio 1.52, 95% confidence interval 1.34-1.73). The number of years of experience in dermatopathology did not significantly influence results.
Main takeaway: Dermatopathologists are swayed by prior diagnoses when consulted for second opinions. They should be blinded to make diagnoses independent from preliminary diagnoses.
Main takeaway: Dermatopathologists are swayed by prior diagnoses when consulted for second opinions. They should be blinded to make diagnoses independent from preliminary diagnoses.
Atopic dermatitis in older adults is correlated with an increased incidence of dementia
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Why dry skin might be more than an annoyance!
Atopic dermatitis, or eczema, is an extremely common dermatological condition that affects 5-15% of those over age 60. Since chronic inflammatory conditions have been linked with dementia, researchers have sought to understand if atopic dermatitis, or eczema, (an inflammatory condition) is associated with an increased risk of dementia.
In this longitudinal cohort study, researchers analyzed data from 1,767,667 patients aged 60-99 from The Health Improvement Network in the United Kingdom. Patients were included if they did not have a previous diagnosis of dementia, but had been diagnosed and treated for atopic dermatitis. Researchers also graded atopic dermatitis severity as mild, moderate, or severe. The primary outcome of this study was a new diagnosis of dementia during follow-up (patients were followed until death, dementia diagnosis, age 105, discontinuance of medical records, or study termination). Results showed that the incidence of dementia was 57 per 10,000 person-years among those with atopic dermatitis and 44 per 10,000 person-years in those without, which represents a 27% increased risk of dementia (hazard ratio, 1.27; 95% CI, 1.23-1.30). The strength of this correlation increased with increased atopic dermatitis severity. Limitations include missing data for socioeconomic status, alcohol use, and tobacco use.
Main Takeaway: This retrospective study found a small but increased risk of dementia in patients with atopic dermatitis.
Atopic dermatitis, or eczema, is an extremely common dermatological condition that affects 5-15% of those over age 60. Since chronic inflammatory conditions have been linked with dementia, researchers have sought to understand if atopic dermatitis, or eczema, (an inflammatory condition) is associated with an increased risk of dementia.
In this longitudinal cohort study, researchers analyzed data from 1,767,667 patients aged 60-99 from The Health Improvement Network in the United Kingdom. Patients were included if they did not have a previous diagnosis of dementia, but had been diagnosed and treated for atopic dermatitis. Researchers also graded atopic dermatitis severity as mild, moderate, or severe. The primary outcome of this study was a new diagnosis of dementia during follow-up (patients were followed until death, dementia diagnosis, age 105, discontinuance of medical records, or study termination). Results showed that the incidence of dementia was 57 per 10,000 person-years among those with atopic dermatitis and 44 per 10,000 person-years in those without, which represents a 27% increased risk of dementia (hazard ratio, 1.27; 95% CI, 1.23-1.30). The strength of this correlation increased with increased atopic dermatitis severity. Limitations include missing data for socioeconomic status, alcohol use, and tobacco use.
Main Takeaway: This retrospective study found a small but increased risk of dementia in patients with atopic dermatitis.
Examining the use of artificial intelligence to assist in the diagnosis of skin cancer
Journal of Investigative Dermatology
Journal of Investigative Dermatology
Who needs artificial intelligence when we have so much natural foolishness?
Just kidding! But in this article, researchers evaluated whether artificial intelligence (AI) could help improve diagnostic accuracy of skin cancers by non-dermatologists. Attending physicians, dermatology residents, and non-dermatology trainees were split into two groups: one that had access to real-time help from an AI algorithm (n=295) and one that did not have access (n=281). Each participant examined 576 cases of suspicious lesions. The authors found that:
Limitations of this study include that although the AI program was intended to help general practitioners in the primary care setting decide when to refer a patient, this study was conducted in a tertiary care center. Additionally, this study was conducted only in the Asian population.
Main Takeaway: AI algorithms significantly improved the diagnostic accuracy of non-dermatology trainees in identifying skin cancers. However, additional studies need to be conducted to determine whether the findings from this study may carry over into clinical practice.
Just kidding! But in this article, researchers evaluated whether artificial intelligence (AI) could help improve diagnostic accuracy of skin cancers by non-dermatologists. Attending physicians, dermatology residents, and non-dermatology trainees were split into two groups: one that had access to real-time help from an AI algorithm (n=295) and one that did not have access (n=281). Each participant examined 576 cases of suspicious lesions. The authors found that:
- The AI-assisted groups were more accurate than the non-assisted groups (53.9% v 43.8%, p=0.019)
- This difference was significant when the user had less exposure to dermatology (non-dermatology trainees) whereas it was not significant with dermatology residents
- The AI program helped expand the working differential
- However, the accuracy of trainees in the AI-assisted group suffered when the AI algorithm provided incorrect predictions
Limitations of this study include that although the AI program was intended to help general practitioners in the primary care setting decide when to refer a patient, this study was conducted in a tertiary care center. Additionally, this study was conducted only in the Asian population.
Main Takeaway: AI algorithms significantly improved the diagnostic accuracy of non-dermatology trainees in identifying skin cancers. However, additional studies need to be conducted to determine whether the findings from this study may carry over into clinical practice.
Clinical and Dermoscopic Evaluation of Trichloroacetic Acid 20% Versus Long-Pulsed 1064-nm Nd-YAG Laser in the Treatment of Keratosis Pilaris
Dermatologic Surgery
Dermatologic Surgery
Peeling good, like I should.
Keratosis Pilaris (KP) is a common disorder of keratinization (think rough bumps on the upper arms and thighs!). Unfortunately, KP is very tough to treat as well. In this split-body randomized clinical trial, researchers sought to evaluate the efficacy of trichloroacetic acid 20% (TCA) chemical peels and long-pulsed Nd:YAG laser in treating KP.
20 female patients were evaluated that had symmetrically distributed areas treated with either the peel or the laser. Investigator Global Assessment showed that 8 patients (40%) had excellent improvement of the laser-treated area and 11 patients (55%) had excellent improvement of TCA-treated area. In the Nd:YAG laser group, 2 patients reported moderate satisfaction with treatment, 13 reported marked satisfaction, and 5 reported excellent satisfaction. In the TCA group, 10 patients reported marked satisfaction and 10 reported excellent satisfaction with the results. Overall, all 20 patients noted improvement in their keratosis pilaris whether they received TCA 20% peel or Nd:YAG laser, with slightly higher mean satisfaction scores for the TCA group. Dermoscopic evaluation yielded equal improvement.
Main Takeaway: All patients were satisfied with improvement seen in their keratosis pilaris whether they received the trichloroacetic acid peel or the Nd:YAG laser.
Keratosis Pilaris (KP) is a common disorder of keratinization (think rough bumps on the upper arms and thighs!). Unfortunately, KP is very tough to treat as well. In this split-body randomized clinical trial, researchers sought to evaluate the efficacy of trichloroacetic acid 20% (TCA) chemical peels and long-pulsed Nd:YAG laser in treating KP.
20 female patients were evaluated that had symmetrically distributed areas treated with either the peel or the laser. Investigator Global Assessment showed that 8 patients (40%) had excellent improvement of the laser-treated area and 11 patients (55%) had excellent improvement of TCA-treated area. In the Nd:YAG laser group, 2 patients reported moderate satisfaction with treatment, 13 reported marked satisfaction, and 5 reported excellent satisfaction. In the TCA group, 10 patients reported marked satisfaction and 10 reported excellent satisfaction with the results. Overall, all 20 patients noted improvement in their keratosis pilaris whether they received TCA 20% peel or Nd:YAG laser, with slightly higher mean satisfaction scores for the TCA group. Dermoscopic evaluation yielded equal improvement.
Main Takeaway: All patients were satisfied with improvement seen in their keratosis pilaris whether they received the trichloroacetic acid peel or the Nd:YAG laser.