FIFTIETH ISSUE
December 27th, 2023
Is there an increased chance of acne in patients taking JAK inhibitors?
JAMA Dermatology
Getting “JAK’ed” takes on a new meaning…
The use of JAK inhibitors to treat dermatologic disease has increased significantly over the past few years. With its increased use, acne vulgaris has been noted as a common adverse effect of JAK inhibitor use. This systematic review and meta-analysis aimed to analyze the risk of acne as an adverse effect to JAK inhibitor use using 25 Phase 2 and 3 randomized controlled trials that included 10,839 participants.
What did they find?
Limitations: Some relevant studies may have been inappropriately excluded. Results are limited to the original limitations of the studies included. Some instances of acne may have been misdiagnosed. Improvements in pre-existing acne are not noted.
Main Takeaway: There is increased risk of developing acne after starting JAK inhibitors. Patients should be adequately counseled on the risk of developing acne before beginning treatment with JAK inhibitors.
The use of JAK inhibitors to treat dermatologic disease has increased significantly over the past few years. With its increased use, acne vulgaris has been noted as a common adverse effect of JAK inhibitor use. This systematic review and meta-analysis aimed to analyze the risk of acne as an adverse effect to JAK inhibitor use using 25 Phase 2 and 3 randomized controlled trials that included 10,839 participants.
What did they find?
- Experimental group patients were 3.83 times more likely to develop acne compared to placebo
- Pooled OR 3.83 [95% CI, 2.76-5.32])
- Pooled OR 3.83 [95% CI, 2.76-5.32])
- Certain JAK inhibitors had a greater association development of acne
- abrocitinib 13.47 [95% CI, 3.25-55.91]
- baricitinib 4.96 [95% CI, 2.52-9.78]
- Upadacitinib 4.79 [95% CI, 3.61-6.37]
- deucravacitinib 2.64 [95%CI, 2.52-9.78]
- deuruxolitinib 3.30 [95% CI, 1.22-8.93]
- abrocitinib 13.47 [95% CI, 3.25-55.91]
Limitations: Some relevant studies may have been inappropriately excluded. Results are limited to the original limitations of the studies included. Some instances of acne may have been misdiagnosed. Improvements in pre-existing acne are not noted.
Main Takeaway: There is increased risk of developing acne after starting JAK inhibitors. Patients should be adequately counseled on the risk of developing acne before beginning treatment with JAK inhibitors.
Hyperbaric oxygen therapy for the treatment of calciphylaxis
journal of the american academy of dermatology
In(heal) deeper… improving calciphylaxis one breath at a time!
Calciphylaxis is a thrombotic vasculopathy characterized by painful necrotic ulcerations of the skin and soft tissue, leading to high morbidity and mortality. While there are currently no FDA-approved treatments for calciphylaxis, IV sodium thiosulfate (IV STS) has traditionally been used as first-line therapy. The combination of hyperbaric oxygen therapy (HBOT) with IV STS has been suggested to enhance wound healing due to HBOT’s ability to improve host defenses and increase tissue oxygenation.
This retrospective cohort study (n = 93) sought to compare outcomes in patients treated with HBOT + IV STS vs. those treated with IV STS only. Primary outcomes were all-cause mortality, mortality due to calciphylaxis, and wound healing of the main lesion.
What did they find?
Main Takeaway: Full HBOT treatment in conjunction with IV STS improved mortality and wound healing calciphylaxis.
Calciphylaxis is a thrombotic vasculopathy characterized by painful necrotic ulcerations of the skin and soft tissue, leading to high morbidity and mortality. While there are currently no FDA-approved treatments for calciphylaxis, IV sodium thiosulfate (IV STS) has traditionally been used as first-line therapy. The combination of hyperbaric oxygen therapy (HBOT) with IV STS has been suggested to enhance wound healing due to HBOT’s ability to improve host defenses and increase tissue oxygenation.
This retrospective cohort study (n = 93) sought to compare outcomes in patients treated with HBOT + IV STS vs. those treated with IV STS only. Primary outcomes were all-cause mortality, mortality due to calciphylaxis, and wound healing of the main lesion.
What did they find?
- HBOT was associated with a significantly longer survival time than the standard treatment (p = 0.016)
- Increased number of HBOT sessions was associated with improved mortality outcomes with session increases predicting hazard ratios
- 1 session HR 0.961(95% CI, 0.911-0.999)
- 5 session HR 0.819 (95% CI, 0.628-0.996)
- 10 session HR 0.671 (95% CI, 0.394-0.993)
- 20 session HR 0.451 (95% CI, 0.155-0.985)
- 1 session HR 0.961(95% CI, 0.911-0.999)
- There was a significant positive relationship between increasing the number of HBOT treatment sessions and wound healing score, with wound healing score increasing by 0.03 units for every additional HBOT treatment session (p = 0.042)
- The most common adverse effect associated with HBOT was anxiety or claustrophobia (22.2%)
Main Takeaway: Full HBOT treatment in conjunction with IV STS improved mortality and wound healing calciphylaxis.
How does HS management differ between dermatologists and non-dermatology providers?
PEdiatric dermatology
Steering clear of the surgical route
Hidradenitis suppurativa (HS) is a chronic skin condition characterized by inflammation, scarring, and occlusion of hair follicles, commonly affecting areas such as the axilla and genital regions. While dermatologists play a key role in treatment escalation, utilizing topical therapies, oral medications, biologics, and multimodal approaches to improve outcomes, non-dermatologist clinicians also play an important role in HS management. This retrospective cohort study aimed to understand the presentation, management, and outcomes of 195 pediatric HS patients (under age 20), comparing outcomes of patients primarily treated by dermatologists vs. other providers.
What did they find?
Main Takeaways: The study suggests an increased likelihood of medical management in dermatology-managed patients with HS, suggesting that surgery may be avoided with optimal medical management and highlighting how educating non-dermatology providers on HS care can improve disease management.
Hidradenitis suppurativa (HS) is a chronic skin condition characterized by inflammation, scarring, and occlusion of hair follicles, commonly affecting areas such as the axilla and genital regions. While dermatologists play a key role in treatment escalation, utilizing topical therapies, oral medications, biologics, and multimodal approaches to improve outcomes, non-dermatologist clinicians also play an important role in HS management. This retrospective cohort study aimed to understand the presentation, management, and outcomes of 195 pediatric HS patients (under age 20), comparing outcomes of patients primarily treated by dermatologists vs. other providers.
What did they find?
- Most patients (76.1%) were seen by dermatology at least once, with referrals often coming from pediatrics (43.2%) and family medicine (15.1%)
- There was a higher prevalence of family history of HS in dermatology-managed patients (17.1% vs. 4.3%), and a higher prevalence of dermatologic comorbidities, particularly acne (36.1% vs. 8.5%), in the dermatology-managed group
- The dermatology-managed group were more likely to have documentation of Hurley stage (46.9% vs. 12.0%) and of key morphologic features, including inflammatory nodules (44.2% vs. 19.1%) and scarring (39.5% vs. 8.5%) from their most recent visit
- Dermatology-managed patients exhibited higher rates of axillary (51.0% vs. 27.7%) and groin involvement (30.6% vs. 8.5%)
- Medication usage was significantly different, with dermatology-managed patients more likely to use chlorhexidine gluconate, benzoyl peroxide, doxycycline, and topical clindamycin
- Dermatology-managed patients were also more likely to be prescribed topicals (83.6% vs. 31.3%), oral antibiotics (53.7% vs. 12.5%), and other systemic treatments (27.6% vs. 3.1%), including biologics (19.7% vs 0%)
- Dermatology-managed patients were less likely to undergo surgical excision and had a longer median duration of management (7.3 vs. 0.77 months)
Main Takeaways: The study suggests an increased likelihood of medical management in dermatology-managed patients with HS, suggesting that surgery may be avoided with optimal medical management and highlighting how educating non-dermatology providers on HS care can improve disease management.
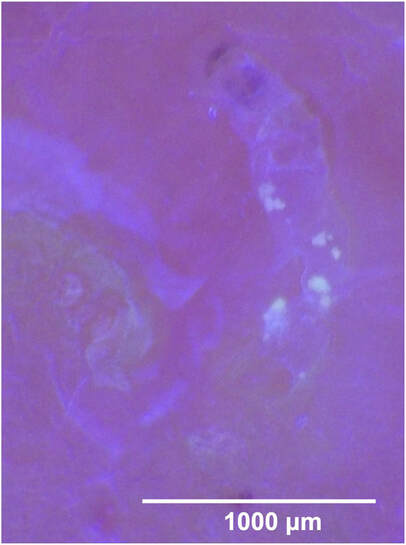
“MITEy” cool way to look and learn more about Scabies
Innovations in Dermatology
Sarcoptes scabiei, otherwise known as scabies, is a mite that thrives in the stratum corneum of human skin where they burrow and lay eggs. Diagnosis is made via clinical presentation. It is hypothesized that ultraviolet A light may allow visualization of endogenous and exogenous fluorescence patterns, enabling scabies mites and burrows to be detected in vivo; this may allow researchers to better understand the life cycle of scabies mites.
What did they find?
What did they find?
- Scabies burrows may be visualized with the application of Ultraviolet A light; this light source may further clarify the traits of the burrows
- The mite feces were visualized as a yellowish deposit within the burrow under Ultraviolet A light
- The Sarcoptes scabiei body and eggs were visualized more clearly in the burrow at increased magnification in ultraviolet light compared to white light
Main Takeaway: Ultraviolet A light with dermatoscope can be an effective tool for visualizing Sarcoptes scabiei.
student spotlight
MY NAME IS VICTORIA SLAVINSKY AND I’M A MEDICAL STUDENT AT GEORGETOWN UNIVERSITY SCHOOL OF MEDICINE CURRENTLY COMPLETING A RESEARCH YEAR IN CTCL AT JOHNS HOPKINS SCHOOL OF MEDICINE.
Chronic solar ultraviolet radiation exposure and increased incidence of non-melanoma skin cancer - a call to action
Nonmelanoma skin cancers remain highly prevalent among the U.S. population, with approximately 90% attributed to cumulative solar radiation (sUVR) exposure. Outdoor workers including those in construction, agriculture, military, and postal workers, are particularly vulnerable to such cancers.
A PubMed-based systematic literature review was performed to address questions regarding UV radiation measurement, the utility of the UV index, and the prevalence of solar lentigines and NMSCs in individuals with outdoor occupations.
What did we find?
Limitations:
The role of individual patient characteristics like family history of skin cancer, Fitzpatrick skin type, number of moles, and history of sunburns in adolescence need to be considered and improved methods for sUVR measurement are required.
Main Takeaway: This evidence-based assessment substantiates the need for improved counseling and educational campaigns on promoting sun-protective behaviors among individuals with outdoor occupations. Regular implementation of practices like wearing protective clothing, wide-brimmed hats, UV protective sunglasses, and the avoidance of peak UV intensity hours is essential.
A PubMed-based systematic literature review was performed to address questions regarding UV radiation measurement, the utility of the UV index, and the prevalence of solar lentigines and NMSCs in individuals with outdoor occupations.
What did we find?
- Outdoor workers often face sUVR that surpasses safety thresholds for occupational settings.
- Their cumulative lifetime UVR exposure is higher, leading to increased prevalence of NMSCs and precursor lesions.
Limitations:
The role of individual patient characteristics like family history of skin cancer, Fitzpatrick skin type, number of moles, and history of sunburns in adolescence need to be considered and improved methods for sUVR measurement are required.
Main Takeaway: This evidence-based assessment substantiates the need for improved counseling and educational campaigns on promoting sun-protective behaviors among individuals with outdoor occupations. Regular implementation of practices like wearing protective clothing, wide-brimmed hats, UV protective sunglasses, and the avoidance of peak UV intensity hours is essential.