ELEVENTH ISSUE
June 1st, 2022
Nonmelanoma Skin Cancer in Patients Older than Age 85 Years Presenting for Mohs Surgery
JAMA Dermatology
In this multicenter cohort study of patients > 85 years old, Maisel-Campbell et al. examined characteristics of elderly patients referred for Mohs surgery.
The main findings include:
Are we harming more than helping our elderly patients with Mohs surgery for nonmelanoma skin cancers? In our elderly population, it has been suggested that Mohs surgery for skin cancer may lead to unnecessary risk and discomfort when weighed against life expectancy and functional status. Maisel-Campbell et al. conducted a multicenter, prospective cohort study to examine the characteristics of patients >85 years old who received Mohs surgery for nonmelanoma skin cancer. In this study, 6.9% of patients presenting for Mohs were over the age of 85. They found that patients who received Mohs were more likely to have facial tumors and higher functional status than those who did not receive Mohs. Some of the main reasons surgeons turn to Mohs include: 1) patient desire for high cure rate (66%), 2) high functional status (57%), and 3) high-risk tumor types (40.2%). The findings of this study suggest that patient functional status may play a role in deciding how cancers are treated. Overall, Mohs surgery can be appropriate for some older patients, especially since our elderly population may have unique barriers to care (limited social support, increased burden of repeat or self-applied treatments). However, future studies are required to better understand patient preference, identify in which patient populations surgery would be most beneficial, and to define what nonsurgical options would be the most appropriate alternatives when surgery is not preferable.
The main findings include:
- Patients who received Mohs surgery were more likely to have facial tumors and high functional status for their age, compared to patients who did not receive Mohs surgery
- Surgeons who proceed with Mohs frequently cite a patient desire for high cure rate, high patient functional status, and high-risk tumor type as reasons for surgery
- Mohs may be appropriate in some older patients, especially since they may have unique barriers to care (limited social support, increased burden of repeat or self-applied treatments)
Are we harming more than helping our elderly patients with Mohs surgery for nonmelanoma skin cancers? In our elderly population, it has been suggested that Mohs surgery for skin cancer may lead to unnecessary risk and discomfort when weighed against life expectancy and functional status. Maisel-Campbell et al. conducted a multicenter, prospective cohort study to examine the characteristics of patients >85 years old who received Mohs surgery for nonmelanoma skin cancer. In this study, 6.9% of patients presenting for Mohs were over the age of 85. They found that patients who received Mohs were more likely to have facial tumors and higher functional status than those who did not receive Mohs. Some of the main reasons surgeons turn to Mohs include: 1) patient desire for high cure rate (66%), 2) high functional status (57%), and 3) high-risk tumor types (40.2%). The findings of this study suggest that patient functional status may play a role in deciding how cancers are treated. Overall, Mohs surgery can be appropriate for some older patients, especially since our elderly population may have unique barriers to care (limited social support, increased burden of repeat or self-applied treatments). However, future studies are required to better understand patient preference, identify in which patient populations surgery would be most beneficial, and to define what nonsurgical options would be the most appropriate alternatives when surgery is not preferable.
How does microneedling improve the efficacy of melasma treatment?
Journal of the American Academy of Dermatology
Journal of the American Academy of Dermatology
Melasma is not just a “pregnancy mask”. Melasma refers to a disorder of hypermelanosis that typically presents on the face. While melasma disproportionately affects skin of color females, it is present in the general population with a prevalence as high as 1.5% to 33%. Unfortunately, treatment of melasma remains very difficult. This systematic review analyzes the efficacy of microneedling as an adjuvant to topical therapies in treating melasma.
Melasma is not just a “pregnancy mask.” Melasma refers to a disorder of hypermelanosis that typically presents on the face. While melasma disproportionately affects skin of color females, it is present in the general population with a prevalence as high as 1.5% to 33%. Unfortunately, treatment of melasma remains very difficult with photoprotection and lightening agents (such as hydroquinones) as our first line agents. Other treatment options include lasers, mechanical and chemical peels, and oral tranexamic acid (TXA). Recently, microneedling, which is a procedure that creates tiny microporations in the skin, has shown efficacy for melasma, however the reproducibility of results and side effects of the procedure has yet to be examined. This systematic review analyzes the efficacy of microneedling as an adjuvant to topical therapies in treating melasma.
What did they find?
Limitations include that there was some concern of bias in the studies included and that there was no way to determine how microneedling type and depth of penetration impacted efficacy. Overall, microneedling as an adjunct to topical therapies provides a safe way to improve melasma management, with maximal impact seen at 12 weeks
- 12 studies were included: 5 were randomized controlled trials, 2 were randomized split face studies, and 5 were nonrandomized split face studies
- Topical therapy + microneedling resulted in additional improvement at 8 weeks with moderate effect and large effect at 12-16 weeks (standardized mean difference 1.04, 95% CI 0.6-1.48)
- Microneedling alone resulted in improvement in melasma severity, demonstrating 23%-29% improvement in 2 months
- Microneedling was well tolerated, with common side effects including transient burning, itching and erythema; mild post-inflammatory dyspigmentation was reported in 5%-12% in some studies
Melasma is not just a “pregnancy mask.” Melasma refers to a disorder of hypermelanosis that typically presents on the face. While melasma disproportionately affects skin of color females, it is present in the general population with a prevalence as high as 1.5% to 33%. Unfortunately, treatment of melasma remains very difficult with photoprotection and lightening agents (such as hydroquinones) as our first line agents. Other treatment options include lasers, mechanical and chemical peels, and oral tranexamic acid (TXA). Recently, microneedling, which is a procedure that creates tiny microporations in the skin, has shown efficacy for melasma, however the reproducibility of results and side effects of the procedure has yet to be examined. This systematic review analyzes the efficacy of microneedling as an adjuvant to topical therapies in treating melasma.
What did they find?
- 12 studies were included: 5 were randomized controlled trials, 2 were randomized split face studies, and 5 were nonrandomized split face studies
- Topical therapy + microneedling resulted in additional improvement at 8 weeks with moderate effect and large effect at 12-16 weeks (standardized mean difference 1.04, 95% CI 0.6-1.48)
- Microneedling alone resulted in improvement in melasma severity, demonstrating 23%-29% improvement in 2 months
- Microneedling was well tolerated, with common side effects including transient burning, itching and erythema; mild post-inflammatory dyspigmentation was reported in 5%-12% in some studies
Limitations include that there was some concern of bias in the studies included and that there was no way to determine how microneedling type and depth of penetration impacted efficacy. Overall, microneedling as an adjunct to topical therapies provides a safe way to improve melasma management, with maximal impact seen at 12 weeks
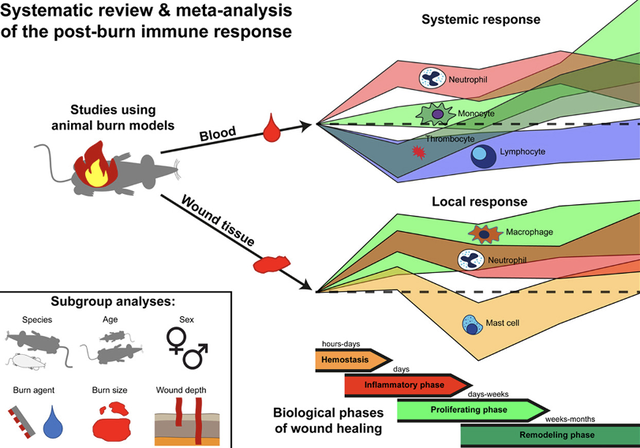
Using animal studies to better understand the immune response to burn injury
Journal of Investigative Dermatology
Journal of Investigative Dermatology
Systemic inflammatory response syndrome is a pathophysiological response that may occur after severe burn, which can result in organ failure and death. Our understanding of the immunologic response to burn is limited. To improve our knowledge, a systematic review of the inflammatory response to burn in animals was performed.
‘Cause I’m burnin’ up, burnin’ up for *understanding the immunologic response to burn* babyyyyy. Systemic inflammatory response syndrome is a pathophysiological response that may occur after severe burn, in severe cases resulting in organ failure or death. Our understanding of the immunologic response to burn injury is limited. While studies on the human response to burn exist in medical literature, they are difficult to standardize because reported cases have varying sample collection times and different degrees of injury. To improve our knowledge, a systematic review of the inflammatory response to burn in animals was performed. 247 animal studies were included in this study, highlighting 14 immune cell responses to burn; these studies were standardized and included before and after burn skin sampling. It was found that peripheral blood had increased numbers of neutrophils, monocytes and thrombocytes within the first week of injury, which remains high up to a month post-burn. Lymphocyte counts, however, are reduced in the first two weeks after injury. Together, these results indicate that the innate response is involved in the immediate burn response. It was found that the burn response had an increased migration of leukocytes, and that antibacterial activity of neutrophils was reduced during days 5-9 after injury. This study is limited in that it was performed on animals, and while they allow for a better understanding of immune response overall, undoubtedly more research must be done into the immune response in humans. This study is significant because it improves our understanding of the immune response to burn injury and may be influential in improving our burn care and outcomes moving forward.
- 247 animal studies were included, which identified the immune response to burn in 14 different immune cell types
- Increased numbers of neutrophils, monocytes and thrombocytes are seen in the burn wound tissue in the first week after injury
- Lymphocyte counts are reduced two weeks after injury
- Antibacterial activity of neutrophils was reduced during days 5-9 after injury
- Innate immune response is involved in the immediate burn response
‘Cause I’m burnin’ up, burnin’ up for *understanding the immunologic response to burn* babyyyyy. Systemic inflammatory response syndrome is a pathophysiological response that may occur after severe burn, in severe cases resulting in organ failure or death. Our understanding of the immunologic response to burn injury is limited. While studies on the human response to burn exist in medical literature, they are difficult to standardize because reported cases have varying sample collection times and different degrees of injury. To improve our knowledge, a systematic review of the inflammatory response to burn in animals was performed. 247 animal studies were included in this study, highlighting 14 immune cell responses to burn; these studies were standardized and included before and after burn skin sampling. It was found that peripheral blood had increased numbers of neutrophils, monocytes and thrombocytes within the first week of injury, which remains high up to a month post-burn. Lymphocyte counts, however, are reduced in the first two weeks after injury. Together, these results indicate that the innate response is involved in the immediate burn response. It was found that the burn response had an increased migration of leukocytes, and that antibacterial activity of neutrophils was reduced during days 5-9 after injury. This study is limited in that it was performed on animals, and while they allow for a better understanding of immune response overall, undoubtedly more research must be done into the immune response in humans. This study is significant because it improves our understanding of the immune response to burn injury and may be influential in improving our burn care and outcomes moving forward.
QUESTION OF THE WEEK
NEJM CHALLENGE QUESTION
A 30-year-old man with Crohn’s disease presented to the dermatology clinic with multiple painful ulcers in his groin and perineal area, as well as an ongoing Crohn’s disease flare with fatigue, abdominal pain, and bloody diarrhea. Physical examination of the skin showed deep, linear erosions across the perineum and inguinal folds, on the scrotum and penile shaft, and in the intergluteal cleft. Which of the following is the most likely etiology underlying the genital ulcers?
1. Ecthyma gangrenosum
2. Knife-cut ulcers from Crohn’s disease
3. Lichen sclerosis
4. Linear IgA disease
5. Pemphigus foliaceous
1. Ecthyma gangrenosum
2. Knife-cut ulcers from Crohn’s disease
3. Lichen sclerosis
4. Linear IgA disease
5. Pemphigus foliaceous
Answer: Knife-cut ulcers from Crohn’s disease
Physical examination of the skin showed deep, linear erosions across the perineum and inguinal folds, on the scrotum and penile shaft, and in the intergluteal cleft. Skin swabs were negative for infections, including bacterial, fungal, herpes simplex viral, and tubercular infections. A diagnosis of “knife-cut” ulcers resulting from Crohn’s disease was made. These ulcers are a cutaneous manifestation of Crohn’s disease in which noncaseating, granulomatous inflammation is observed on skin biopsy that is similar to that observed on gastrointestinal biopsy. Adalimumab was prescribed, and at follow-up at 4 weeks, both the gastrointestinal symptoms and the skin lesions had cleared.
Other answers:
1. Ecthyma gangrenosum- although these lesions do commonly occur in the anogenital area (and extremities), typically presents as an ulcer with necrotic black eschar secondary to pseudomonas aeruginosa infection. Patients are often immunosuppressed or neutropenic
3. Lichen sclerosus- although lichen sclerosus (aka LS&A) typically presents in genital region (85% of time), the classic presentation includes sclerotic, ivory-white, atrophic and flat-topped papules coalescing into plaques
4. Linear IgA disease- blistering disorder that presents with tense vesicles/bullae and urticarial plaques in annular, polycyclic, or herpetiform (“crown of jewels”) arrangement. What antigens are the target for linear IgA disease? LAD-1 and LABD-97, which are both derived from BPAG2 (BP180)- the same antigenic target in bullous pemphigoid!
5. Pemphigus foliaceous - superficial blistering disorders caused by autoantibodies targeting desmoglein 1; presents with impetigo-like crusted erosions that leave a “cornflake” scale. Favors the seborrheic distribution
Explanations developed with use of Alikhan, Ali, and Thomas LH Hocker. Review of Dermatology E-Book. Elsevier Health Sciences, 2017.
Physical examination of the skin showed deep, linear erosions across the perineum and inguinal folds, on the scrotum and penile shaft, and in the intergluteal cleft. Skin swabs were negative for infections, including bacterial, fungal, herpes simplex viral, and tubercular infections. A diagnosis of “knife-cut” ulcers resulting from Crohn’s disease was made. These ulcers are a cutaneous manifestation of Crohn’s disease in which noncaseating, granulomatous inflammation is observed on skin biopsy that is similar to that observed on gastrointestinal biopsy. Adalimumab was prescribed, and at follow-up at 4 weeks, both the gastrointestinal symptoms and the skin lesions had cleared.
Other answers:
1. Ecthyma gangrenosum- although these lesions do commonly occur in the anogenital area (and extremities), typically presents as an ulcer with necrotic black eschar secondary to pseudomonas aeruginosa infection. Patients are often immunosuppressed or neutropenic
3. Lichen sclerosus- although lichen sclerosus (aka LS&A) typically presents in genital region (85% of time), the classic presentation includes sclerotic, ivory-white, atrophic and flat-topped papules coalescing into plaques
4. Linear IgA disease- blistering disorder that presents with tense vesicles/bullae and urticarial plaques in annular, polycyclic, or herpetiform (“crown of jewels”) arrangement. What antigens are the target for linear IgA disease? LAD-1 and LABD-97, which are both derived from BPAG2 (BP180)- the same antigenic target in bullous pemphigoid!
5. Pemphigus foliaceous - superficial blistering disorders caused by autoantibodies targeting desmoglein 1; presents with impetigo-like crusted erosions that leave a “cornflake” scale. Favors the seborrheic distribution
Explanations developed with use of Alikhan, Ali, and Thomas LH Hocker. Review of Dermatology E-Book. Elsevier Health Sciences, 2017.
SK(IN DEPTH) RECAP
In Ao et al., they found that systemic steroids + ________ shortened clinical duration of Steven Johnson Sundrome and Toxic Epidermal Necrolysis.
A. Mycophenolate Mofetil
B. Hydroxychloroquine
C. Etanercept
D. Secukinumab
E. Benralizumab
What TNF-alpha inhibitor is a fully human monoclonal IgG antibody against the transmembrane TNF-receptor?
A. Adalimumab
B. Infliximab
C. Etanercept
What is the dominant mutation for small congenital melanocytic nevi?
A. Fumarate hydratase
B. BRCA1 associated protein 1
C. BRAFV600E
A. Mycophenolate Mofetil
B. Hydroxychloroquine
C. Etanercept
D. Secukinumab
E. Benralizumab
What TNF-alpha inhibitor is a fully human monoclonal IgG antibody against the transmembrane TNF-receptor?
A. Adalimumab
B. Infliximab
C. Etanercept
What is the dominant mutation for small congenital melanocytic nevi?
A. Fumarate hydratase
B. BRCA1 associated protein 1
C. BRAFV600E
In Ao et al., they found that systemic steroids + ________ shortened clinical duration of Steven Johnson Sundrome and Toxic Epidermal Necrolysis.
A. Mycophenolate Mofetil
B. Hydroxychloroquine
C. Etanercept
D. Secukinumab
E. Benralizumab
Patients treated with a combination of steroids and etanercept had shorter courses of initial steroid usage, acute stage of disease, skin healing time, and hospitalization. Additionally, they found that patients treated with the combination had lower levels of specific cytokines compared to the steroid only group.
What TNF-alpha inhibitor is a fully human monoclonal IgG antibody against the transmembrane TNF-receptor?
A. Adalimumab
B. Infliximab
C. Etanercept
Adalimumab is the correct answer. Infliximab is a chimeric monoclonal IgG antibody binding TNF-a only. Etanercept is a fully human dimeric fusion protein that binds both TNF-a and TNF-b.
What is the dominant mutation for small congenital melanocytic nevi?
A. Fumarate hydratase
B. BRCA1 associated protein 1
C. BRAFV600E
In Dong et al., they found that Opsin 3 physically interacts with BRAFV600E to affect melanogenesis in congenital melanocytic nevus cells. Knocking down OPN3 inhibited signaling pathways that ultimately increased melanin levels in congenital melanocytic cells. These studies suggest a role for OPN3 in melanogenesis in congenital melanocytic nevus. Fumarate hydratase mutations are associated with Hereditary Leiomyomatosis and Renal Cell Carcinoma. BRCA1 associated protein 1 mutations are associated with BAP1 tumor predisposition syndrome.
A. Mycophenolate Mofetil
B. Hydroxychloroquine
C. Etanercept
D. Secukinumab
E. Benralizumab
Patients treated with a combination of steroids and etanercept had shorter courses of initial steroid usage, acute stage of disease, skin healing time, and hospitalization. Additionally, they found that patients treated with the combination had lower levels of specific cytokines compared to the steroid only group.
What TNF-alpha inhibitor is a fully human monoclonal IgG antibody against the transmembrane TNF-receptor?
A. Adalimumab
B. Infliximab
C. Etanercept
Adalimumab is the correct answer. Infliximab is a chimeric monoclonal IgG antibody binding TNF-a only. Etanercept is a fully human dimeric fusion protein that binds both TNF-a and TNF-b.
What is the dominant mutation for small congenital melanocytic nevi?
A. Fumarate hydratase
B. BRCA1 associated protein 1
C. BRAFV600E
In Dong et al., they found that Opsin 3 physically interacts with BRAFV600E to affect melanogenesis in congenital melanocytic nevus cells. Knocking down OPN3 inhibited signaling pathways that ultimately increased melanin levels in congenital melanocytic cells. These studies suggest a role for OPN3 in melanogenesis in congenital melanocytic nevus. Fumarate hydratase mutations are associated with Hereditary Leiomyomatosis and Renal Cell Carcinoma. BRCA1 associated protein 1 mutations are associated with BAP1 tumor predisposition syndrome.